慢性疼痛的抗菌治疗(第1部分):镇痛机制。
IF 3.4
3区 医学
Q2 CLINICAL NEUROLOGY
引用次数: 0
摘要
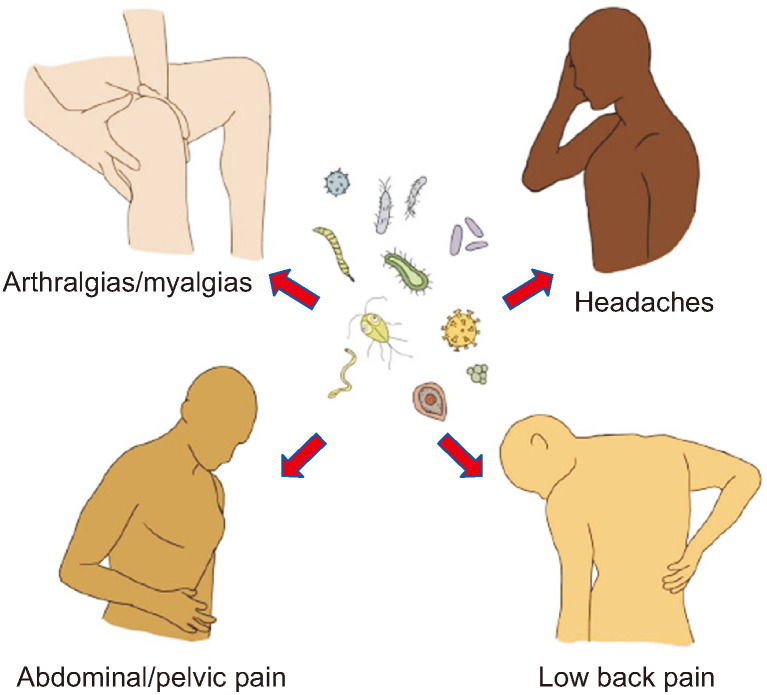
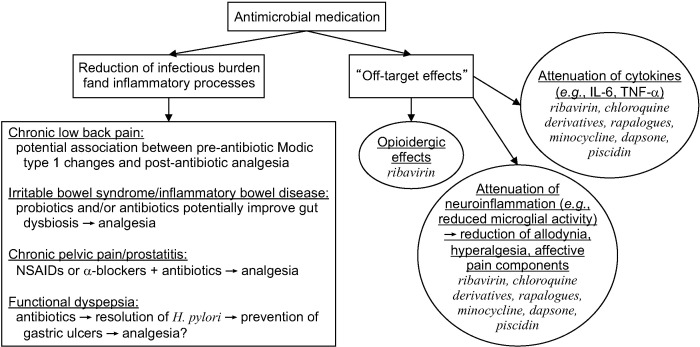
越来越多的证据表明,慢性疼痛和感染之间的关系是复杂而交织在一起的。细菌和病毒感染可通过多种机制引起疼痛,如直接组织损伤和炎症,诱导过度免疫活动以及外周或中枢致敏的发展。治疗感染可能通过减轻这些过程来缓解疼痛,但越来越多的文献表明,一些抗菌疗法具有镇痛作用,包括伤害性和神经性疼痛症状,以及疼痛的情感成分。抗菌药物的镇痛机制是间接的,但可以分为两大类:1)减轻感染负担和相关的促炎过程;2)通过脱靶效应(非预期结合位点)抑制痛觉和适应性不良神经可塑性改变所必需的信号过程(如酶和细胞因子活性)。对于前者,有证据表明慢性腰痛(与Modic 1型改变相关)、肠易激综合征、炎症性肠病、慢性盆腔痛和功能性消化不良的症状可能在抗生素治疗后得到改善,尽管关于具体方案和剂量以及哪些亚群最有可能受益的问题仍然存在。对于后者,有证据表明,几种抗菌药物和药物具有独立于其减少感染负担的镇痛作用,其中包括头孢菌素、利巴韦林、氯喹衍生物、雷帕罗酮、米诺环素、氨苯砜和鱼毒素-1。本文旨在全面综述现有文献中临床前或临床研究中已证明具有镇痛作用的抗菌药物。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Antimicrobial therapies for chronic pain (part 1): analgesic mechanisms.
There is increasing evidence that the relationship between chronic pain and infections is complex and intertwined. Bacterial and viral infections can cause pain through numerous mechanisms such as direct tissue damage and inflammation, the induction of excessive immunologic activity, and the development of peripheral or central sensitization. Treating infections might relieve pain by attenuating these processes, but a growing body of literature suggests that some antimicrobial therapies confer analgesic effects, including for nociceptive and neuropathic pain symptoms, and affective components of pain. The analgesic mechanisms of antimicrobials are indirect, but might be conceptualized into two broad categories: 1) the reduction of the infectious burden and associated pro-inflammatory processes; and 2) the inhibition of signaling processes (e.g., enzymatic and cytokine activity) necessary for nociception and maladaptive neuroplastic changes via off-target effects (unintended binding sites). For the former, there is evidence that symptoms of chronic low back pain (when associated with Modic type 1 changes), irritable bowel syndrome, inflammatory bowel disease, chronic pelvic pain, and functional dyspepsia might be improved after antibiotic treatment, though significant questions remain regarding specific regimens and dose, and which subpopulations are most likely to benefit. For the latter, there is evidence that several antimicrobial classes and medications exert analgesic effects independent of their reduction of infectious burden, and these include cephalosporins, ribavirin, chloroquine derivatives, rapalogues, minocycline, dapsone, and piscidin-1. This article aims to comprehensively review the existing literature for antimicrobial agents that have demonstrated analgesic efficacy in preclinical or clinical studies.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Korean Journal of Pain
Medicine-Anesthesiology and Pain Medicine
CiteScore
5.40
自引率
7.10%
发文量
57
审稿时长
16 weeks
期刊介绍:
Korean Journal of Pain (Korean J Pain, KJP) is the official journal of the Korean Pain Society, founded in 1986. It has been published since 1988. It publishes peer reviewed original articles related to all aspects of pain, including clinical and basic research, patient care, education, and health policy. It has been published quarterly in English since 2009 (on the first day of January, April, July, and October). In addition, it has also become the official journal of the International Spinal Pain Society since 2016. The mission of the Journal is to improve the care of patients in pain by providing a forum for clinical researchers, basic scientists, clinicians, and other health professionals. The circulation number per issue is 50.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


