月经周期相关脑疾病激素临床试验的范围综述:经前情绪障碍、月经期偏头痛和月经期癫痫的研究。
摘要
正常月经周期内激素的周期性变化是多种中枢神经系统(CNS)相关疾病的基础,包括经前情绪障碍(PMD)、月经期偏头痛(MM)和月经期癫痫(CE)。尽管有这种基本的机械联系,但这三个领域相互独立地运作。在这篇范围界定综述(N=85项研究)中,我们调查了PMD、MM和CE中现有的人类研究,以概述在这些领域进行的外源性实验性激素操纵试验。我们检查了这些疾病的广泛文献,以总结现有的诊断实践和研究方法,突出实验人类文献中的空白,并阐明每个领域未来的研究机会。虽然没有一种单独的治疗或研究设计能够适应每种疾病,但在月经周期相关疾病PMD、MM和CE中,研究设计和基于神经内分泌的激素敏感性存在巨大重叠。范围界定综述结构摘要:背景。月经周期可能是某些大脑疾病症状的生物学触发因素,导致与月经周期相关的特定现象,如经前情绪障碍(PMD)、月经偏头痛(MM)和月经期癫痫(CE)。尽管在慢性和激素激发方面存在重叠,但这些领域在历史上一直独立运作,没有任何关于方法或机制的系统交流。目的:使用在线数据库来识别1950年至2021年间发表的研究患有PMD、MM或CE的育龄女性激素操作的文章。我们选择了符合以下标准的N=85项研究:1)包括具有自然月经周期的女性研究人群(例如,非围绝经期、怀孕或使用非主要研究变量的激素药物);2) 涉及外源性激素操作;3) 涉及跨越至少两个周期阶段的重复测量作为主要结果变量。图表方法:在导出在线数据库查询结果后,作者提取了样本量、样本群体的临床诊断、研究设计、实验激素操作、周期性结果测量以及每次试验的结果。图表绘制是手动完成的,每个试验由两名作者审查。结果:与MM(N=21)或CE(N=8)相比,外源性激素操作已被测试为PMD的治疗选择(N=56项试验)。联合口服避孕药(COC)试验,特别是那些含有屈螺酮作为孕激素的试验,是一个研究良好的领域,在治疗PMDD和MM方面都有很好的结果。我们没有在CE中发现COC试验。许多试验使用促性腺激素释放激素激动剂(GnRHa)测试排卵抑制,一项荟萃分析支持其在PMD中的疗效;GnRHa已经在两个MM相关试验和一个CE开放标签病例系列中进行了测试。最后,我们发现非避孕激素操作,包括但不限于短期透皮雌二醇、补充黄体酮和拮抗黄体酮,已用于所有三种疾病。结论:PMD、MM和CE的研究通常有重叠的研究设计和研究方法,一些干预措施的相似效果表明,重叠机制可能导致其周期性症状表现。我们的范围审查是第一次总结这三种大脑疾病的现有临床试验,特别是激素治疗试验。我们发现PMD有大量关于排卵抑制COC和GnRHa试验的文献;MM领域包括广泛的基于雌激素的研究;目前CE的共识集中在黄体期补充孕酮,由于担心癫痫发作,雌激素操作有限。我们认为,在评估、诊断、分型和实验操作方法方面,任何一个学科的研究人员都会从更多的交流中受益。通过这项范围界定综述,我们希望加强研究人员之间的合作和沟通,最终改善与月经周期相关的大脑疾病的诊断和治疗。
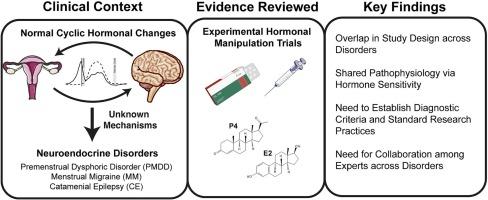
Cyclic variations in hormones during the normal menstrual cycle underlie multiple central nervous system (CNS)-linked disorders, including premenstrual mood disorder (PMD), menstrual migraine (MM), and catamenial epilepsy (CE). Despite this foundational mechanistic link, these three fields operate independently of each other. In this scoping review (N = 85 studies), we survey existing human research studies in PMD, MM, and CE to outline the exogenous experimental hormone manipulation trials conducted in these fields. We examine a broad range of literature across these disorders in order to summarize existing diagnostic practices and research methods, highlight gaps in the experimental human literature, and elucidate future research opportunities within each field. While no individual treatment or study design can fit every disease, there is immense overlap in study design and established neuroendocrine-based hormone sensitivity among the menstrual cycle-related disorders PMD, MM, and CE.
Scoping review structured summary
Background. The menstrual cycle can be a biological trigger of symptoms in certain brain disorders, leading to specific, menstrual cycle-linked phenomena such as premenstrual mood disorders (PMD), menstrual migraine (MM), and catamenial epilepsy (CE). Despite the overlap in chronicity and hormonal provocation, these fields have historically operated independently, without any systematic communication about methods or mechanisms.
Objective. Online databases were used to identify articles published between 1950 and 2021 that studied hormonal manipulations in reproductive-aged females with either PMD, MM, or CE. We selected N = 85 studies that met the following criteria: 1) included a study population of females with natural menstrual cycles (e.g., not perimenopausal, pregnant, or using hormonal medications that were not the primary study variable); 2) involved an exogenous hormone manipulation; 3) involved a repeated measurement across at least two cycle phases as the primary outcome variable.
Charting methods. After exporting online database query results, authors extracted sample size, clinical diagnosis of sample population, study design, experimental hormone manipulation, cyclical outcome measure, and results from each trial. Charting was completed manually, with two authors reviewing each trial.
Results. Exogenous hormone manipulations have been tested as treatment options for PMD (N = 56 trials) more frequently than MM (N = 21) or CE (N = 8). Combined oral contraceptive (COC) trials, specifically those containing drospirenone as the progestin, are a well-studied area with promising results for treating both PMDD and MM. We found no trials of COCs in CE. Many trials test ovulation suppression using gonadotropin-releasing hormone agonists (GnRHa), and a meta-analysis supports their efficacy in PMD; GnRHa have been tested in two MM-related trials, and one CE open-label case series. Finally, we found that non-contraceptive hormone manipulations, including but not limited to short-term transdermal estradiol, progesterone supplementation, and progesterone antagonism, have been used across all three disorders.
Conclusions. Research in PMD, MM, and CE commonly have overlapping study design and research methods, and similar effects of some interventions suggest the possibility of overlapping mechanisms contributing to their cyclical symptom presentation. Our scoping review is the first to summarize existing clinical trials in these three brain disorders, specifically focusing on hormonal treatment trials. We find that PMD has a stronger body of literature for ovulation-suppressing COC and GnRHa trials; the field of MM consists of extensive estrogen-based studies; and current consensus in CE focuses on progesterone supplementation during the luteal phase, with limited estrogen manipulations due to concerns about seizure provocation. We argue that researchers in any of these respective disciplines would benefit from greater communication regarding methods for assessment, diagnosis, subtyping, and experimental manipulation. With this scoping review, we hope to increase collaboration and communication among researchers to ultimately improve diagnosis and treatment for menstrual-cycle-linked brain disorders.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


