Use of Anti-epileptic Drugs for Post Traumatic Seizure: A Global Survey.
IF 1.8
Q4 NEUROSCIENCES
引用次数: 0
Abstract
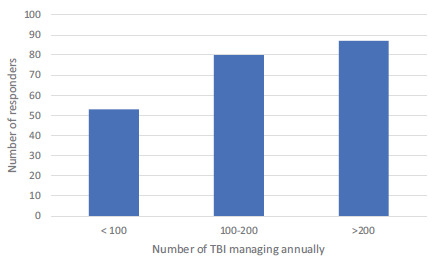
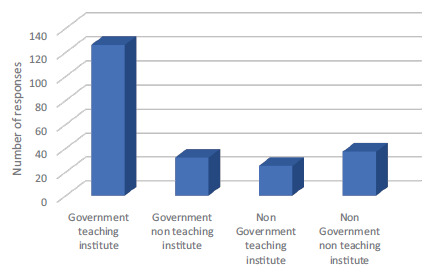
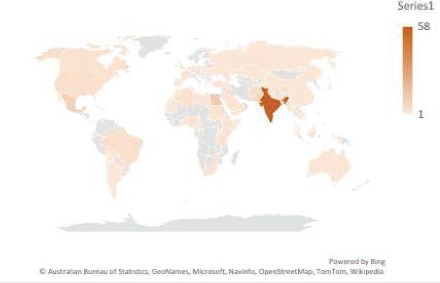
Background Post traumatic seizures (PTS) and post traumatic epilepsy (PTE) are potential consequences of traumatic brain injury (TBI). There is no consensus regarding its management among treating doctors. Purpose We have undertaken a global survey to assess the variability of management practices of PTS and PTE and highlight the pressing need to formulate uniform practice guidelines. Methods A questionnaire consisting of sixteen questions were developed with the help of Google survey and sent through e-mail, or social media platforms like WhatsApp, Facebook messenger or Telegram, to practicing Neurologists and Neurosurgeons round the world. Results There were a total of 220 responses. Majority of our responders (n = 202; 91.8%) would start an anti-epileptic (AED) prophylaxis to prevent PTS; 18 people (8.18%) told that they would not start AED prophylaxis for TBI. Phenytoin (n = 98; 48.5%) followed by Levetiracetam (n = 78; 38.6%) was the preferred drug, although the latter was significantly preferred by high and upper middle-income countries (p<.001). Majority (n = 99; 49%) would not use it beyond two weeks. Most clinicians would manage PTE with a single drug (n = 160; 72.7%) either Phenytoin (n = 69; 31.3%) or levetiracetam (n = 67; 30.4%). Most of them (n = 174; 86%) would treat for less than one year. Conclusions Practices in the management of PTS and PTE vary widely among clinicians. Our study point towards the need for the development of a more robust and comprehensive practice guidelines for the management of the same.
抗癫痫药物在创伤后癫痫发作中的应用:一项全球调查。
背景:创伤后癫痫发作(PTS)和创伤后癫痫(PTE)是创伤性脑损伤(TBI)的潜在后果。治疗医生对其管理没有共识。目的:我们进行了一项全球调查,以评估PTS和PTE管理实践的可变性,并强调制定统一实践指南的迫切需要。方法:在谷歌调查的帮助下,开发了一份由16个问题组成的问卷,并通过电子邮件或WhatsApp, Facebook messenger或Telegram等社交媒体平台发送给世界各地的执业神经科医生和神经外科医生。结果:共收到220份问卷。大多数应答者(n = 202;91.8%)会开始抗癫痫(AED)预防PTS;18人(8.18%)表示他们不会因TBI而开始AED预防。苯妥英(n = 98;48.5%),其次是左乙拉西坦(n = 78;38.6%)是首选药物,尽管后者在高收入和中高收入国家明显更受欢迎(p001)。多数(n = 99;49%)不会使用超过两周。大多数临床医生会用单一药物治疗PTE (n = 160;72.7%)或苯妥英(n = 69;31.3%)或左乙拉西坦(n = 67;30.4%)。大多数(n = 174;86%)愿意接受不到一年的治疗。结论:临床医生对PTS和PTE的治疗方法差异很大。我们的研究指向需要制定一套更为健全和全面的管理实践指南。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


