Late consequences of masked bioprosthetic valve endocarditis: diagnostic and treatment options.
IF 0.6
Q4 SURGERY
引用次数: 0
Abstract
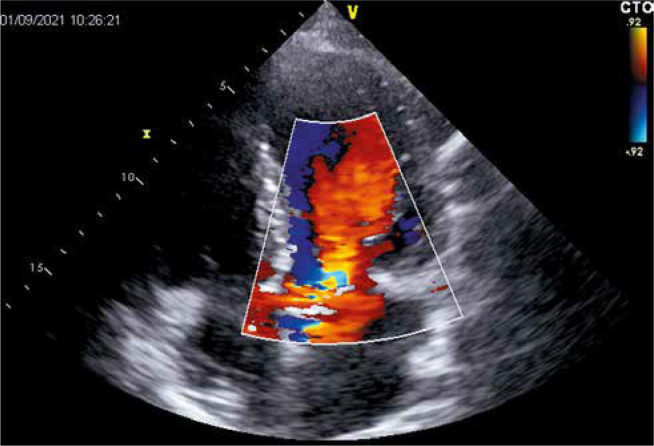
Address for correspondence: Dominika Katarzyńska MD, University Clinical Hospital, Poznan, Poland, e-mail: dominika.katarzynska@gmail.com Received: 12.05.2023, accepted: 25.06.2023. A 77-year-old male patient presented with heart failure symptoms (NYHA class III), which developed after probable infective endocarditis (IE) a few months earlier. Physical examination revealed new heart murmur and peripheral oedema. His other medical history includes hypertension, laryngeal tumor, and spine surgery. Nine years prior to this presentation, he was qualified for surgical aortic valve replacement (SAVR) due to a symptomatic severe aortic stenosis with mild aortic regurgitation. After sternotomy, he was deferred from prosthesis implantation as the porcelain aorta was revealed. Subsequently, he underwent successful transcatheter aortic valve implantation (TAVI) with Medtronic CoreValve 29 mm (Medtronic, Minneapolis, MN, USA) bioprosthesis. Postprocedural transthoracic echocardiography (TTE) showed proper bioprosthesis function with maximal transaortic gradient of 25 mm Hg without a paravalvular leak (PVL). The postoperative course was uneventful and on the 7th day he was discharged home. Three weeks after the procedure, the patient developed recurrent syncope, dizziness and chest pain. Electrocardiogram showed severe bradycardia with periodic third-degree atrioventricular block. A dual chamber pacemaker (BiotronicEcuro DR, Biotronik, Berlin, Germany) was implanted. During next 9 years the patient remained in a good clinical condition, though he underwent successful treatment of laryngeal tumor. The repeated echocardiographic examination confirmed proper bioprosthesis function. Six months before current hospitalization he presented with infection which was interpreted as pneumonia and treated successfully with antibiotics. Nevertheless, thereafter symptoms of heart failure occurred and gradually exacerbated. During the hospitalization due to heart failure worsening, TTE revealed hemodynamically severe intraprosthetic aortic regurgitation which had not been observed before (confirmed in transesophageal echocardiography (TEE) (Figure 1)) with transaortic maximal and mean gradients of 21 and 10 mm Hg, respectively, preserved left ventricular ejection fraction, and increased pulmonary artery systolic pressure. Laboratory tests did not present significant deviations in inflammatory markers and blood cultures were negative. After careful assessment by the heart team the patient was qualified for valve-in-valve TAVI (ViV-TAVI) due to a high perioperative risk and porcelain aorta. After careful assessment of computed tomography, he underwent successful uncomplicated implantation of Edwards Sapien (Edwards Lifesciences Corp., Irvine, CA, USA) prosthesis, which was chosen based on its optimal profile not limiting access to the coronary ostia. During follow-up he remains asymptomatic with good prosthesis function on control echocardiography. IE post-TAVI is not a common but serious complication with high in-hospital mortality, which is estimated at about 11–64% and 1-year mortality of 22–75% [1]. The overall incidence of IE post-TAVI is about 1% to 6% [2]. The rate of IE post-TAVI 1 year after surgery ranges from 0.5% to 3.1% and will increase as the procedure gains popularity and the operated patients are older and with a high Late consequences of masked bioprosthetic valve endocarditis: diagnostic and treatment options
隐蔽性生物瓣膜心内膜炎的晚期后果:诊断和治疗选择。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
0.90
自引率
14.30%
发文量
44
审稿时长
6-12 weeks
期刊介绍:
Polish Journal of Thoracic and Cardiovascular Surgery is a quarterly aimed at cardiologists, cardiosurgeons and thoracic surgeons. Includes the original works (experimental, research and development), illustrative and casuistical works about cardiology and cardiosurgery.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


