The changing landscape of cerebral revascularization surgery: A United Kingdom experience.
引用次数: 0
Abstract
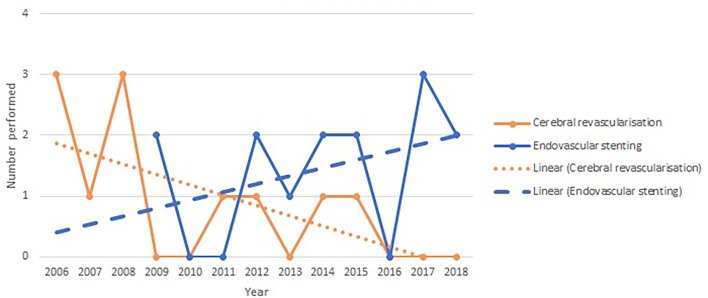
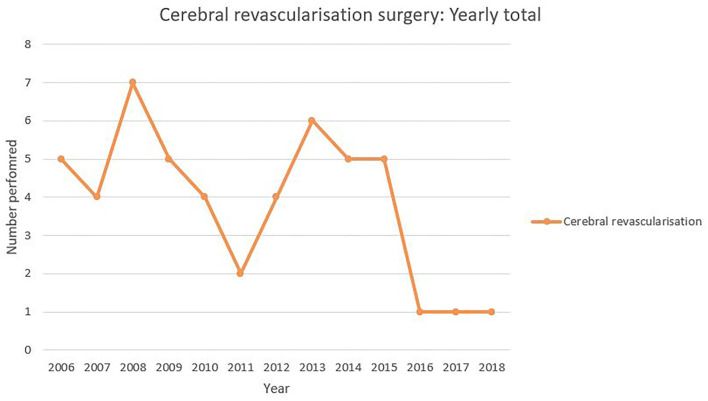
Objective We describe the chronological trends in cerebral revascularization surgery through a single-surgeon experience; and we review whether in the context of giant and fusiform cerebral aneurysms, flow-diverting stents have impacted on the use of cerebral revascularization surgery. Methods We review our single institution prospectively collected database of cerebral revascularization procedures between 2006 and 2018. Comparing this to our database of flow-diverting endovascular stent procedures, we compare the treatment of fusiform and giant aneurysms. We describe patient demographics, procedural incidence, complications, and outcomes. Results Between 2006 and 2018, 50 cerebral revascularization procedures were performed. The incidence of cerebral revascularization surgery is declining. In the context of giant/fusiform aneurysm treatment, the decline in cerebral revascularization is accompanied by a rise in the use of flow-diverting endovascular stents. Thirty cerebral revascularizations were performed for moyamoya disease and 11 for giant/fusiform aneurysm. Four (14%) direct bypass grafts occluded without neurological sequela. Other morbidity included hydrocephalus (2%), transient ischemic attacks (2%), and ischemic stroke (2%). There was one procedure-related mortality (2%). Flow-diverting stents were inserted for seven fusiform and seven giant aneurysms. Comparing the treatment of giant/fusiform aneurysms, there was no significant difference in morbidity and mortality between cerebral revascularization and flow-diverting endovascular stents. Conclusion We conclude that with the decline in the incidence of cerebral revascularization surgery, there is a need for centralization of services to allow high standards and outcomes to be maintained.
脑血运重建术的变化:英国经验。
目的:我们通过单个外科医生的经验描述脑血运重建术的时间趋势;我们回顾了在巨大和梭状脑动脉瘤的背景下,血流转移支架是否影响了脑血运重建术的使用。方法:我们回顾了2006年至2018年间单一机构前瞻性收集的脑血运重建术数据库。将此与我们的血流转移血管内支架手术数据库进行比较,我们比较了梭状动脉瘤和巨动脉瘤的治疗。我们描述了患者的人口统计学特征、手术发生率、并发症和结果。结果:2006年至2018年间,进行了50例脑血运重建术。脑血运重建术的发生率正在下降。在巨大/梭状动脉瘤治疗的背景下,脑血运重建术的下降伴随着血流转移血管内支架的使用的增加。烟雾病30例,巨大/梭状动脉瘤11例。4例(14%)直接旁路移植物闭塞,无神经系统后遗症。其他发病率包括脑积水(2%)、短暂性脑缺血发作(2%)和缺血性脑卒中(2%)。手术相关死亡1例(2%)。7个梭状动脉瘤和7个巨动脉瘤置入分流支架。对比巨/梭状动脉瘤的治疗,脑血运重建术和分流血管内支架的发病率和死亡率无显著差异。结论:随着脑血运重建术发生率的下降,有必要将服务集中起来,以保持高标准和高疗效。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


