The environmental impact of inhaler replacement: A carbon footprint and economic calculation of the National Database of Health Insurance Claims in Japan
Abstract
Background
Drugs are a major source of greenhouse gas (GHG) emissions from healthcare systems. Pressurized metered-dose inhalers (pMDIs) have raised concerns over their environmental impact due to GHG emissions. Evaluations and reduction strategies for GHGs have been primarily studied in Europe, but not in other regions, including Japan. Therefore, our objective was to calculate the carbon footprint of inhalers in Japan and evaluate their reduction scenarios.
Methods
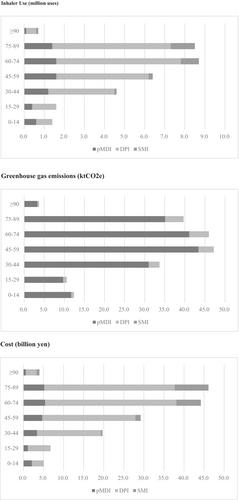
Using the National Database of Health Insurance Claims, our analysis was conducted on inhaler prescriptions in Japan for the fiscal year of 2019. We calculated the number of inhalers used, GHG emissions, and total costs. Next, we simulated the environmental and economic impacts of three reduction scenarios: the first scenario replaced pMDI with dry power inhalers, followed by age-based replacements. In the last scenario, we replaced pMDI with a propellant with a lower global warming potential.
Results
All inhaler-related GHG emissions were 202 ktCO2e, of which 90.9% were attributed to pMDI use. Scenario analysis demonstrated that replacing 10% pMDI with DPI would reduce emissions by 6.7%, with a relatively modest increase in cost; substituting 10% of pMDI used by adults (excluding children and older adults) with alternative inhalers would reduce emissions by 6.1%, with a 0.7% increase in cost; and, replacing 10% of pMDI propellants with lower global warming potential would reduce emissions by 9.3%.
Conclusions
Selecting appropriate inhalers can mitigate GHG emissions in Japan, but its impact will be less than in other countries. Nevertheless, collaborative efforts between physicians, patients, and pharmaceutical companies are necessary to reduce GHG emissions.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


