Persistent high blood pressure and renal dysfunction in preterm infants during childhood
IF 3.1
3区 医学
Q1 PEDIATRICS
引用次数: 0
Abstract
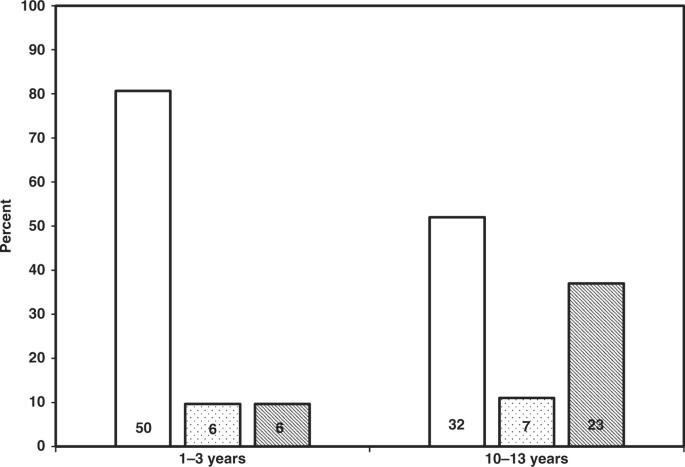
Infants born very preterm (≤32 weeks gestational age, GA) and very-low birth weight (≤1500 g; PT-VLBW) demonstrate high systolic blood pressure (SBP), renal dysfunction, and obesity at 6 months–3 years and in early adulthood. Their parallel measurement and progression during childhood is unclear. We reenrolled 62/120 patients originally seen at 1–3 years at 10–13 years and remeasured anthropometric indices, SBP, and serum creatinine (Cr) and cystatin C (cysC) to determine estimated glomerular filtration rate (eGFR). We selected Term-matched Controls at 10–13 years from the 2015–2016 NHANES database at a ratio of 2 Controls:1 Case (124:62). Reenrolled patients were predominantly Hispanic, birth weight 1073 ± 251 g, and GA at birth 28 ± 2 weeks. At 10–13 years, 45% were classified overweight/obese, 48% had SBP ≥ 90th centile (77% considered hypertensive), and 34% had low eGFR (<90 mL min−1 [1.73 m2]−1). Notably, 57% of reenrolled PT-VLBW Cases had low eGFRcysC at both 1–3 and 10–13 years, P < 0.03. Compared to Controls, Cases had four times the adjusted odds for having an elevated SBP and low eGFRCr despite similar proportions with overweight/obesity among Cases and Controls. PT-VLBW infants seen at 1–3 years exhibit obesity, elevated SBP, and low eGFR in infancy and 10–13 years. Although the small sample size may limit conclusions, pediatricians should consider serial evaluations of PT-VLBW throughout childhood.
早产儿儿童期的持续高血压和肾功能障碍
极早产儿(胎龄≤32 周)和极低出生体重儿(体重≤1500 克;PT-VLBW)在 6 个月至 3 岁以及成年早期表现出高收缩压(SBP)、肾功能障碍和肥胖。他们在儿童期的平行测量和进展情况尚不清楚。我们对 62/120 名最初在 1-3 岁时就诊的患者在 10-13 岁时进行了重新登记,并重新测量了人体测量指数、SBP、血清肌酐 (Cr) 和胱抑素 C (cysC),以确定估计肾小球滤过率 (eGFR)。我们从 2015-2016 年 NHANES 数据库中选取了 10-13 岁的终末匹配对照组,比例为 2 个对照组:1 个病例(124:62)。重新登记的患者主要为西班牙裔,出生体重为 1073±251 g,出生时体重为 28±2 周。在 10-13 岁时,45% 的患者被归类为超重/肥胖,48% 的患者 SBP≥ 第 90 百分位数(77% 被视为高血压),34% 的患者 eGFR 偏低(<90 mL min-1 [1.73 m2]-1)。值得注意的是,57% 的再次入组 PT-VLBW 病例在 1-3 年和 10-13 年的 eGFRcysC 均较低,P <0.03。与对照组相比,尽管病例和对照组中超重/肥胖的比例相似,但病例的调整后 SBP 升高和 eGFRCr 偏低的几率是对照组的四倍。1-3 岁的 PT-VLBW 婴儿在婴儿期和 10-13 岁时表现出肥胖、SBP 升高和 eGFR 低。虽然样本量较小可能会限制结论的得出,但儿科医生应考虑在整个儿童期对 PT-VLBW 进行连续评估。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Pediatric Research
医学-小儿科
CiteScore
6.80
自引率
5.60%
发文量
473
审稿时长
3-8 weeks
期刊介绍:
Pediatric Research publishes original papers, invited reviews, and commentaries on the etiologies of children''s diseases and
disorders of development, extending from molecular biology to epidemiology. Use of model organisms and in vitro techniques
relevant to developmental biology and medicine are acceptable, as are translational human studies
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


