The correlation between different ultrasound planes and computed tomography measures of abdominal aortic aneurysms
Abstract
Introduction
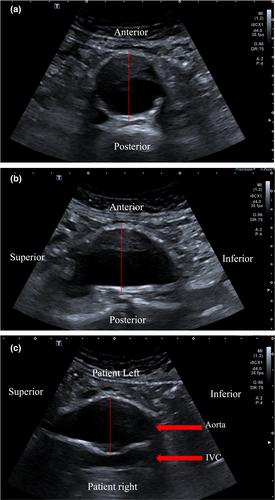
Ultrasound measurements of the aorta are typically taken in the axial plane, with the transducer perpendicular to the aorta, and diameter measurements are obtained by placing the callipers from the anterior to the posterior wall and the transverse right to the left side of the aorta. While the ‘conventional’ anteroposterior walls in both sagittal and transverse plains may be suitable for aneurysms with less complicated geometry, there is controversy regarding the suitability of this approach for complicated, particularly tortuous aneurysms, as they may offer a more challenging situation. Previous work undertaken within our research group found that when training inexperienced users of ultrasound, they demonstrated more optimal calliper placement to the abdominal aorta when approached from a decubitus window to obtain a coronal image compared to the traditional ultrasound approach.
Purpose
To observe the level of agreement in real-world reporting between computed tomography (CT) and ultrasound measurements in three standard planes; transverse AP, sagittal AP and coronal (left to right) infra-renal abdominal aortic aneurysm (AAA) diameter.
Methodology
This is a retrospective review of the Otago Vascular Diagnostics database for AAA, where ultrasound and CT diameter data, available within 90 days of each other, were compared. In addition to patient demographics, the infrarenal aorta ultrasound diameter measurements in transverse AP and sagittal AP, along with a coronal decubitus image of the aorta was collected. No transverse measurement was performed from the left to the right of the aorta.
Results
Three hundred twenty-five participants (238 males, mean age 76.4 ± 7.5) were included. Mean ultrasound outer to the outer wall, transverse AP and sagittal AP diameters were 48.7 ± 10.5 mm and 48.9 ± 9.9 mm, respectively. The coronal diameter measurement of the aorta from left to right was 53.9 ± 12.8 mm in the left decubitus window. The mean ultrasound max was 54.3 ± 12.6 mm. The mean CT diameter measurement was 55.6 ± 12.7 mm. Correlation between the CT max and ultrasound max was r2 = 0.90, and CT with the coronal measurement r2 = 0.90, CT and AP transverse was r2=0.80, and CT with AP sagittal measurement was r2 = 0.77.
Conclusion
The decubitus ultrasound window of the abdominal aorta, with measurement of the coronal plane, is highly correlated and in agreement with CT scanning. This window may offer an alternative approach to measuring the infrarenal abdominal aortic aneurysm and should be considered when performing surveillance of all infra-renal AAA.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


