Quadratus Lumborum Blockade for Postoperative Analgesia in Infants and Children Following Colorectal Surgery.
引用次数: 1
Abstract
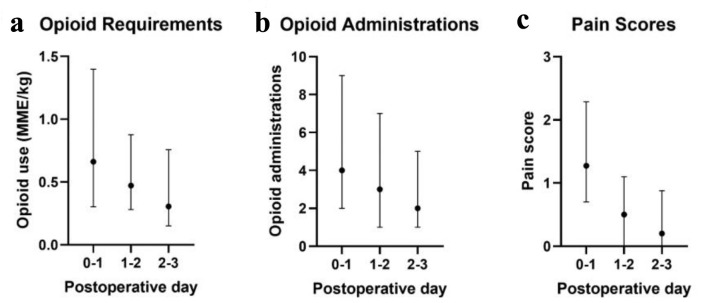
Background Adult studies have indicated that the quadratus lumborum block (QLB) may provide superior analgesia compared to single-shot neuraxial and other truncal peripheral nerve blocks. The technique is being increasingly used for postoperative analgesia in children undergoing lower abdominal surgery. To date, these pediatric reports have been limited by small sample sizes, which may hinder the interpretation of results and assessment of safety. In this study, we retrospectively examined QLBs performed at a large tertiary care hospital for evidence of effectiveness and safety in the pediatric colorectal surgery population. Methods Patients less than 21 years of age who underwent abdominal surgery and received a unilateral or bilateral QLB over a 4-year period were identified in the electronic medical record. Patient demographics, surgery type, and QLB characteristics were retrospectively examined. Pain scores and opioid consumption were tabulated over the first 72-h postoperative period. QLB procedural complications or adverse events attributable to the regional anesthetic were obtained. Results The study cohort included 204 QLBs in 163 pediatric-aged patients (2 days to 19 years of age, median age of 2.4 years). The most common indication was unilateral blockade for ostomy creation or reversal. The majority of QLBs were performed using ropivacaine 0.2% with a median volume of 0.6 mL/kg. The median opioid requirement in oral morphine milligram equivalents (MMEs) was 0.7, 0.5, and 0.3 MME/kg on the first, second, and third postoperative days, respectively. Median pain scores were less than 2 over each time period. Aside from block failure (incidence 1.2%), there were no complications or postoperative adverse events related to the QLBs. Conclusion This retrospective review in a large cohort of pediatric patients demonstrates that the QLB can be performed safely and efficiently in children undergoing colorectal surgery. The QLB provides adequate postoperative analgesia, has a high success rate, may limit postoperative opioid consumption, and is associated with a limited adverse effect profile.
腰方肌阻滞用于婴幼儿结直肠术后镇痛。
背景:成人研究表明,腰方肌阻滞(QLB)可能提供优于单针轴神经阻滞和其他截尾周围神经阻滞。这项技术越来越多地用于儿童下腹部手术的术后镇痛。到目前为止,这些儿科报告受到样本量小的限制,这可能会妨碍对结果的解释和安全性评估。在本研究中,我们回顾性研究了在一家大型三级医疗医院实施的QLBs,以证明其在儿科结直肠手术人群中的有效性和安全性。方法:年龄小于21岁的接受腹部手术并接受单侧或双侧QLB超过4年的患者在电子病历中被识别。回顾性检查患者人口统计学、手术类型和QLB特征。术后72小时内疼痛评分和阿片类药物使用情况制成表格。获得QLB手术并发症或归因于区域麻醉的不良事件。结果:研究队列包括163例儿科年龄患者(2天至19岁,中位年龄2.4岁)的204例QLBs。最常见的指征是单侧阻塞造口或逆转。大多数qlb使用0.2%罗哌卡因进行,中位体积为0.6 mL/kg。术后第1天、第2天和第3天口服吗啡毫克当量(MMEs)的阿片类药物需求量中位数分别为0.7、0.5和0.3 MME/kg。每个时间段的疼痛评分中位数小于2分。除了阻滞失败(发生率1.2%)外,没有与qlb相关的并发症或术后不良事件。结论:这项对大量儿童患者的回顾性研究表明,QLB在接受结直肠手术的儿童中可以安全有效地进行。QLB提供足够的术后镇痛,成功率高,可能限制术后阿片类药物的消耗,并且与有限的不良反应相关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


