Inflammatory related plasma proteins involved in acute preschool wheeze
Abstract
Background
Preschool wheeze is a risk factor for asthma development. However, the molecular mechanism behind a wheezing episode is not well understood.
Objective
Our aims were to assess the association of plasma proteins with acute preschool wheeze and to study the proteins with differential expression at the acute phase at revisit after 3 months. Additionally, to investigate the relationship between protein expression and clinical parameters.
Method
We measured 92 inflammatory proteins in plasma and clinical parameters from 145 children during an episode of preschool wheeze (PW) and at the revisit after 3 months (PW-R, n = 113/145) and 101 healthy controls (HC) aged 6–48 months in the GEWAC cohort using the antibody-mediated proximity extension-based assay (Olink Proteomics, Uppsala).
Results
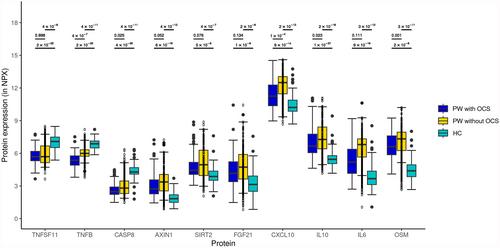
Of the 74 analysed proteins, 52 were differentially expressed between PW and HC. The expression profiles of the top 10 proteins, Oncostatin M (OSM), IL-10, IL-6, Fibroblast growth factor 21 (FGF21), AXIN1, CXCL10, SIRT2, TNFSF11, Tumour necrosis factor β (TNF-β) and CASP8, could almost entirely separate PW from HC. Five out of 10 proteins were associated with intake of oral corticosteroids (OCS) 24 h preceding blood sampling (OSM, CASP8, IL-10, TNF-β and CXCL10). No differences in protein expression were seen between PWs with or without OCS in comparison to HC. At the revisit after 3 months, differential protein expressions were still seen between PW-R and HC for three (IL-10, SIRT2 and FGF21) of the 10 proteins.
Conclusion
Our results contribute to unravelling potential immunopathological pathways shared between preschool wheeze and asthma.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


