COVID-19 and mental health in the UK: Depression, anxiety and insomnia and their associations with persistent physical symptoms and risk and vulnerability factors
Abstract
Objectives
Mental health problems and persistent COVID-19 symptoms were prevalent in the context of COVID-19. However, despite the long-observed association between physical symptoms and mental health problems, such association has not been adequately examined in the context of COVID-19. Our understanding of wider patterns of risk and vulnerability factors for mental health also remains limited. This study investigated the associations between general mental health, and persistent physical symptoms, and additional risk and vulnerability factors in the context of COVID-19.
Methods
Two hundred fourteen adults, living in the UK, recruited via social media, completed the online survey and were included in the analyses. Correlation and regression analyses were conducted to examine the associations of persistent physical symptoms and risk and vulnerability factors with measures of general mental health including depressive symptoms, anxiety and insomnia.
Results
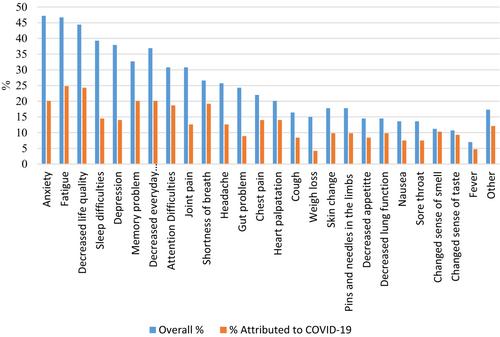
78.5% of the participants reported between 1 and 26 persistent symptoms, and about 28%–92% of them associated these symptoms with COVID-19 infection. Persistent physical symptoms were uniquely associated with all measures of mental health, β = .19–.32. Mental health history and worries were the most prominent risk factors, |β| = .12–.43.
Conclusions
People who experience more persistent physical symptoms post-COVID-19 have poorer mental health. It may be important to consider and discuss the recovery from COVID-19 beyond a negative COVID-19 test. Multidisciplinary interventions that address the complex impact of COVID-19 for people with long COVID are needed.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


