Concordance between patient-reported and physician-documented comorbidities and symptoms among Stage 4 breast cancer patients
Abstract
Background
Comorbidities and symptoms in metastatic breast cancer patients impact treatment decisions and influence prognosis and quality of life. The objective of this study is to examine the concordance between physician documentation and patient reports of comorbidities and symptoms to understand their comparative effectiveness.
Methods
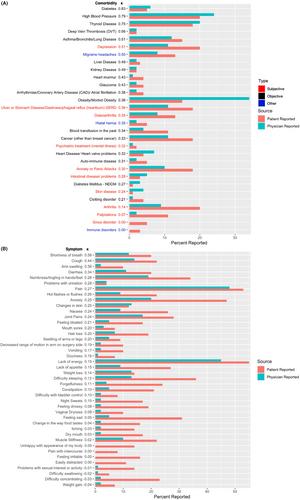
New patients with metastatic breast cancer completed an electronic intake survey assessing patient health history and symptoms. Physician documentation across 54 comorbidities and 42 symptoms was abstracted from notes for the corresponding clinic visits between November 2016 and March 2020. Concordance between patient reports and medical records for each condition and hazards ratios for each patient versus physician reported comorbidity and symptom were assessed.
Results
A total of 168 patients were included in the analysis (age, median = 56 years, range = 29–86 years; 131 white [78.9%]). Twenty-three of 54 comorbidities had a moderate to high level of agreement between patients and physicians (κ ≥ 0.40). Physicians documented higher numbers of comorbidities that can be objectively measured which also had higher concordance (e.g., diabetes [κ = 0.83] and hypertension [κ = 0.79]) while patients reported higher numbers of comorbidities that are more subjective which also had lower concordance (anxiety [κ = 0.30], GERD [κ = 0.36]). One physician-documented and two patient-reported comorbidities were significantly associated with survival (p < 0.05). Only 2 of 42 symptoms had a moderate to high level of agreement between patients and physicians. One physician-documented and nine patient-reported symptoms were significantly associated with decreased survival (p < 0.05).
Conclusion
Agreement between patients' and physicians' reporting of comorbidities varies substantially, and patient reports can complement physician documentation. Physicians significantly underreported symptoms versus patients; thus, concordance was also low. Multiple patient-reported symptoms were predictive of survival; thus, incorporating them can provide more informative estimates of predicted survival.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


