Supporting self-determination in mental health recovery: Strategies employed by occupational therapists
Abstract
Introduction
Self-determination is a core component of mental health recovery and a predictor of positive outcomes. The literature calls for occupational therapists to lead practice change to greater recovery-orientation, including facilitating people's self-determination. However, systemic challenges thwart translation of policy into practice and therapists report a lack of confidence in implementing recovery-oriented principles. This study aimed to understand the strategies that mental health occupational therapists employ to support people's self-determination.
Methods
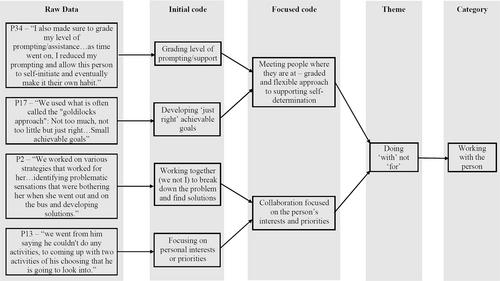
Data were collected through an international on-line questionnaire principally comprising two open-ended questions designed to elicit deep reflective personal accounts. Participants were asked about an experience in which they supported a person's self-determination and the factors that either facilitated or hindered this experience. Qualitative data were analysed using inductive thematic analysis, guided by constant comparative methods.
Findings
Thirty-four therapists, predominantly from Australia (n = 30), participated. Therapists described supporting self-determination as a multifaceted process that involved: (1) working on myself, (2) working with the person, and (3) working with others. They emphasised that the combined use of various strategies across these three areas of work was important to support people's self-determination. Further, awareness of and addressing issues of power in their practice was key.
Conclusion
This study supports the translation of recovery-oriented principles into practice by revealing the nuanced strategies implemented by occupational therapists striving to support self-determination. Participants employed diverse strategies to empower people to take the ‘driver's seat’ in their mental health recovery journey. Insights from this study will support other occupational therapists to actualise recovery-oriented principles and better support self-determination in their practice. To effectively implement self-determination strategies, therapists must reflect on and address existing power differentials within mental health services, particularly between themselves and the people they support.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


