Stability monitoring of patients with myasthenia gravis using a mobile-based application.
IF 0.5
Q4 CLINICAL NEUROLOGY
引用次数: 0
Abstract
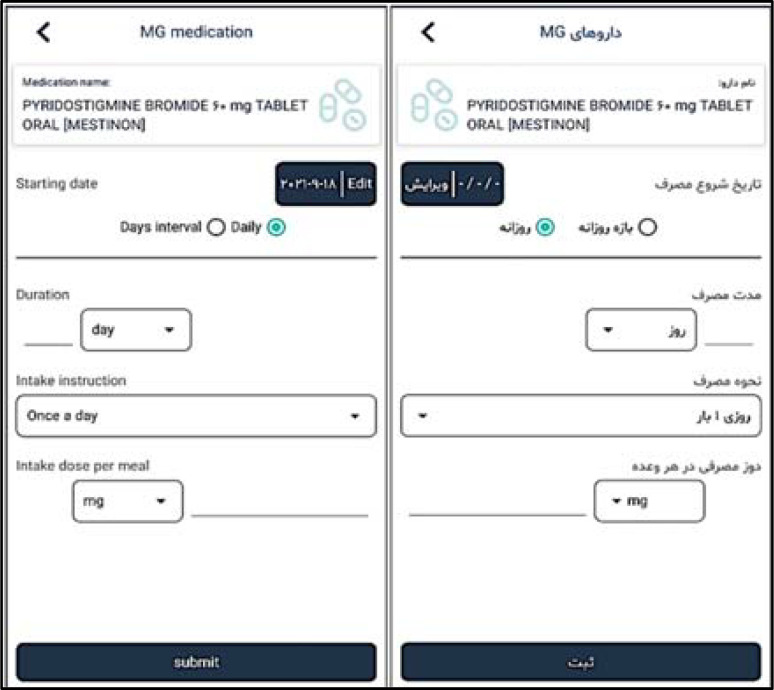
Background: Failure in early diagnosis of myasthenia gravis (MG) and the risks of taking certain medications and undergoing surgery and anesthesia can lead to severe respiratory disorders and death. However, there are therapeutic measures that significantly control the disease and improve individual’s functionality. Methods: First, an expert panel was formed, and a needs assessment questionnaire was prepared for the information elements and the capabilities required for the application and provided to neurologists with a subspecialty fellowship in neuromuscular diseases. Then, based on the analyzed results, the application was designed and created in 2 versions (physician and patient), and in 2 languages (Persian and English). Eventually, a questionnaire for user interaction and satisfaction was provided to 5 relevant physicians to evaluate the application. Results: The results showed that neurologists considered all items of the needs assessment questionnaire to be 100% essential. The capabilities of the application included registering the medication name and dose, recording symptoms and complaints by the patient, completing standard questionnaires, online chat, medication reminder, sending alerts to the doctor when the patient is unwell, and providing a variety of reports. The usability evaluation showed that neurologists evaluated the application at a good level with the average score of 8.23 ± 0.47 (out of 9 points). Conclusion: In the long run, using this technology can reduce costs, improve patients’ quality of life (QOL) and health care, change health behaviors, and ultimately, improve individual’s health.


使用移动应用程序监测重症肌无力患者的稳定性
背景:重症肌无力(MG)的早期诊断失败以及服用某些药物、接受手术和麻醉的风险可导致严重的呼吸系统疾病和死亡。然而,有治疗措施,显著控制疾病和改善个人的功能。方法:首先,组成专家小组,编制需求评估问卷,评估应用所需的信息要素和能力,并提供给神经肌肉疾病亚专科的神经科医师。然后,根据分析结果,设计并创建了2个版本(医生和患者)以及2种语言(波斯语和英语)的应用程序。最终向5位相关医师提供用户交互和满意度问卷,对应用进行评价。结果:神经科医师认为需求评估问卷的所有项目都是100%必要的。该应用程序的功能包括注册药物名称和剂量,记录患者的症状和投诉,完成标准问卷,在线聊天,药物提醒,在患者不舒服时向医生发送警报,以及提供各种报告。可用性评价显示,神经科医师对应用程序的评价处于良好水平,平均得分为8.23±0.47(满分9分)。结论:从长远来看,使用该技术可以降低成本,改善患者的生活质量和医疗保健,改变健康行为,最终改善个人健康。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Current Journal of Neurology
CLINICAL NEUROLOGY-
CiteScore
0.80
自引率
14.30%
发文量
30
审稿时长
12 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


