Excess adiposity and iron-deficient status in Colombian women of reproductive age
Abstract
Objective
Information about excess adiposity markers different from BMI and iron status is limited and more so about the shape of these associations. This study evaluated the relationship between three adiposity markers and iron-deficient status in reproductive-age women.
Methods
Cross-sectional analysis in 6357 non-pregnant women from the Colombian nutritional health survey (ENSIN) 2010. Exposures were the following: waist circumference (WC), waist-to-height ratio (W-HtR), BMI, and WC > 80 cm, W-HtR > 0.5, and BMI ≥ 25 and ≥30. Outcomes were the following: iron deficiency (ID) as serum ferritin <15 μg/L, ID as ferritin <30 μg/L, anemia, and continuous values of ferritin and hemoglobin. Logistic and linear regressions adjusted for sociodemographic/inflammation covariates were conducted.
Results
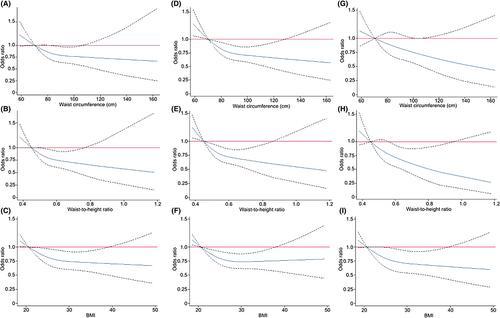
All the adiposity markers, continuous or categorical, were inversely and significantly associated with both ID thresholds in fully adjusted models (p < 0.05). W-HtR reported stronger effect estimates for ID (odds ratios < 0.5) and for prediction of log-ferritin levels (fully adjusted β-coefficient [95% CI] 0.61 [0.39–0.82], p < 0.01) and was also inversely associated with anemia (p < 0.05). In cubic splines analyses, W-HtR, WC, and BMI were linearly associated with ID from values closer to international thresholds of general or central obesity, and the patterns of WC and BMI tended toward flatness. A significant decline in the likelihood of anemia was steeper by increasing W-HtR than by increasing BMI. After exclusion of women with C reactive protein > 5 mg/L or adjustment for C reactive protein, adiposity markers remained significantly related to ferritin levels and W-HtR with anemia.
Conclusions
Women with higher adiposity were less likely to have an iron-deficient status. W-HtR was the strongest and most consistently associated marker. Inflammation would not be involved in the associations found.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


