The effects of COVID-19 on child mental health: Biannual assessments up to April 2022 in a clinical and two general population samples
Abstract
Background
The COVID-19 pandemic has had an acute impact on child mental and social health, but long-term effects are still unclear. We examined how child mental health has developed since the start of the COVID-19 pandemic up to 2 years into the pandemic (April 2022).
Methods
We included children (age 8–18) from two general population samples (N = 222–1333 per measurement and N = 2401–13,362 for pre-covid data) and one clinical sample receiving psychiatric care (N = 334–748). Behavioral questionnaire data were assessed five times from April 2020 till April 2022 and pre-pandemic data were available for both general population samples. We collected parent-reported data on internalizing and externalizing problems with the Brief Problem Monitor and self-reported data on Anxiety, Depressive symptoms, Sleep-related impairments, Anger, Global health, and Peer relations with the Patient-Reported Outcomes Measurement Information System (PROMIS®).
Results
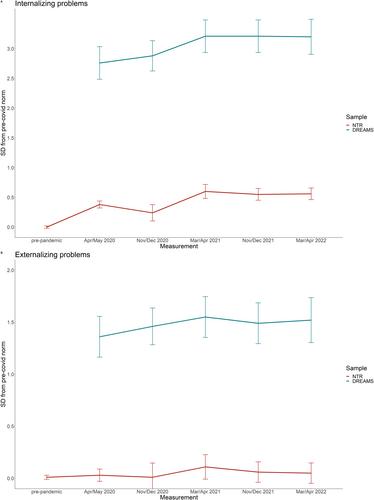
In all samples, parents reported overall increased internalizing problems, but no increases in externalizing problems, in their children. Children from the general population self-reported increased mental health problems from before to during the pandemic on all six PROMIS domains, with generally worst scores in April 2021, and scores improving toward April 2022 but not to pre-pandemic norms. Children from the clinical sample reported increased mental health problems throughout the pandemic, with generally worst scores in April 2021 or April 2022 and no improvement. We found evidence of minor age effects and no sex effects.
Conclusions
Child mental health in the general population has deteriorated during the first phase of the COVID-19 pandemic, has improved since April 2021, but has not yet returned to pre-pandemic levels. Children in psychiatric care show worsening of mental health problems during the pandemic, which has not improved since. Changes in child mental health should be monitored comprehensively to inform health care and policy.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


