Microsatellite Instability with BRAF V600E Associated with Delayed Presentation but Poor Survival in Stage III Colorectal Cancer.
Fortune journal of health sciences
Pub Date : 2023-01-01
Epub Date: 2023-04-19
DOI:10.26502/fjhs.112
引用次数: 0
Abstract
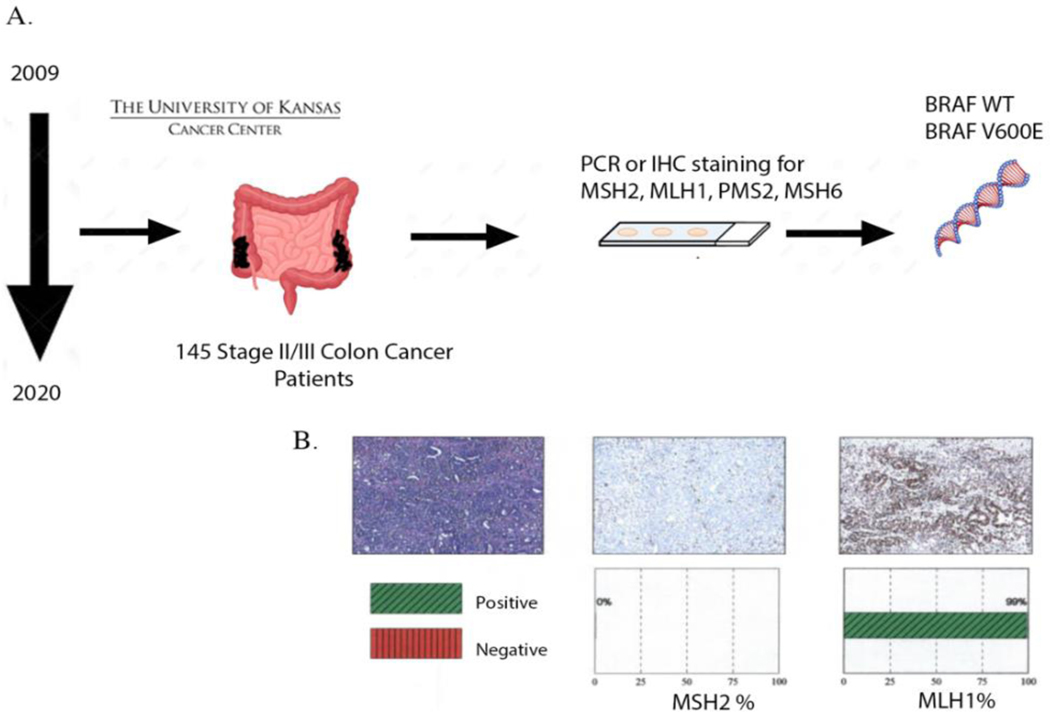
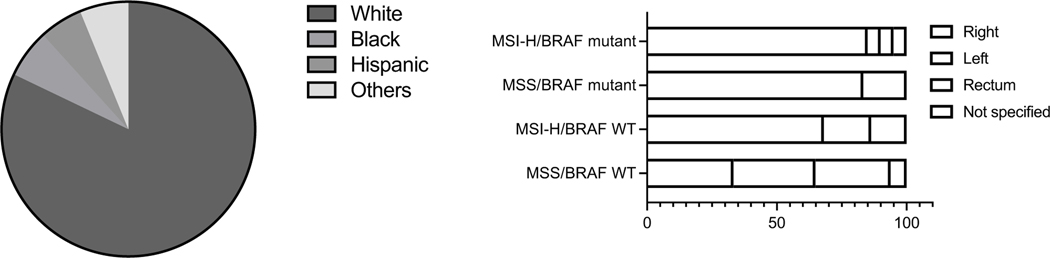
Colorectal cancer (CRC) has tremendous molecular and genetic heterogeneity, making it a difficult cancer to treat. Two of the key prognostic indicators of CRC include microsatellite instability (MSI) and BRAF V600E mutation. Here, we performed a retrospective survival analysis on 145 stage II and III CRC patients treated at the University of Kansas Cancer Center between 2009 and 2020. Of the 145 patients, BRAF V600E was observed in 15% patients and MSI in 28% patients. Median survival was not reached for stage II. For stage III, patients with BRAF V600E showed poor overall survival, which worsened with concurrent presence of MSI [χ2=6.4, p=0.01]. Eighty-five percent of this group was found to have right-sided CRC. For stage III, overall survival (OS) was 27 months, 37 months, 87 months and not reached for MSI-H/BRAF V600E, MSS/BRAF V600E, MSS/BRAF WT and MSI-H/BRAF WT, respectively. Although associated with poor prognosis, presence of MSI in BRAF V600E patients was associated with delayed disease presentation (mean age 77) compared to those with stable microsatellite (mean age 63) [p=0.01]. Although median survival between the groups could not be assessed for stage II due to very few deaths and/or inadequate length of study, comparison of survival trend suggests that BRAF V600E, rather than MSI, is what drives prognosis in stage II CRC. Our findings suggest that prognostic value of MSI is more relevant for stage III than stage II CRC. Patients with MSI-H and BRAF V600E have advantage of late presentation, although at the cost of poor overall prognosis.

BRAF V600E微卫星不稳定性与癌症III期大肠癌的延迟表现但生存率低相关。
结直肠癌癌症(CRC)具有巨大的分子和遗传异质性,是一种难以治疗的癌症。CRC的两个关键预后指标包括微卫星不稳定性(MSI)和BRAF V600E突变。在此,我们对2009年至2020年间在堪萨斯大学癌症中心接受治疗的145名II期和III期CRC患者进行了回顾性生存分析。在145名患者中,15%的患者出现BRAF V600E,28%的患者出现MSI。II期未达到中位生存率。对于III期,BRAF V600E患者的总生存率较差,随着MSI的同时存在而恶化[χ2=6.4,p=0.01]。该组中85%的患者患有右侧CRC。III期的总生存期(OS)分别为27个月、37个月和87个月,MSI-H/BRAF V600E、MSS/BRAF V6 00E、MSS/BRAF WT和MSI-H/BRAF WT未达到。尽管与不良预后相关,但与具有稳定微卫星的患者(平均年龄63岁)相比,BRAF V600E患者中MSI的存在与疾病表现延迟(平均年龄77岁)相关[p=0.01]。尽管由于死亡人数很少和/或研究时间不足,无法评估组间II期的中位生存率,生存趋势的比较表明,BRAF V600E而不是MSI是II期CRC预后的驱动因素。我们的研究结果表明,MSI的预后价值与III期CRC比II期CRC更相关。MSI-H和BRAF V600E患者具有晚期表现的优势,尽管其代价是总体预后不佳。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


