Biological therapies for premature ovarian insufficiency: what is the evidence?
IF 2.3
Q2 PUBLIC, ENVIRONMENTAL & OCCUPATIONAL HEALTH
Frontiers in reproductive health
Pub Date : 2023-09-07
eCollection Date: 2023-01-01
DOI:10.3389/frph.2023.1194575
引用次数: 0
Abstract
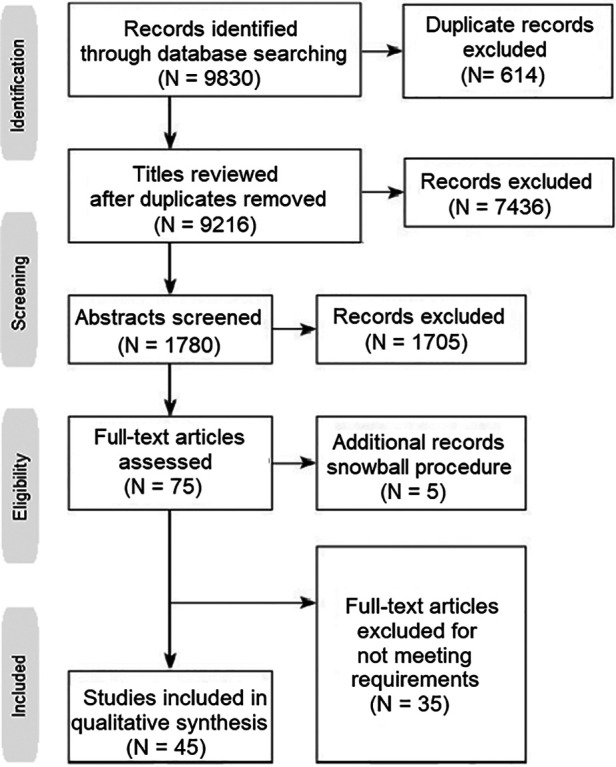
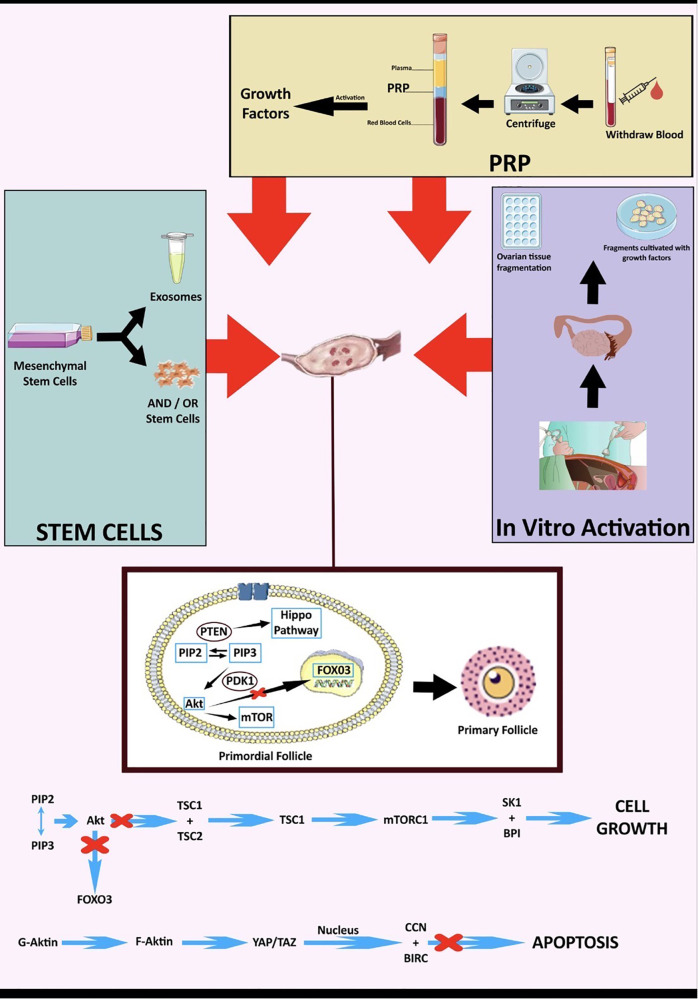
Premature Ovarian Insufficiency (POI) is a multi-factorial disorder that affects women of reproductive age. The condition is characterized by the loss of ovarian function before the age of 40 years and several factors have been identified to be implicated in its pathogenesis. Remarkably though, at least 50% of women have remaining follicles in their ovaries after the development of ovarian insufficiency. Population data show that approximately up to 3.7% of women worldwide suffer from POI and subsequent infertility. Currently, the treatment of POI-related infertility involves oocyte donation. However, many women with POI desire to conceive with their own ova. Therefore, experimental biological therapies, such as Platelet-Rich Plasma (PRP), Exosomes (exos) therapy, In vitro Activation (IVA), Stem Cell therapy, MicroRNAs and Mitochondrial Targeting Therapies are experimental treatment strategies that focus on activating oogenesis and folliculogenesis, by upregulating natural biochemical pathways (neo-folliculogenesis) and improving ovarian microenvironment. This mini-review aims at identifying the main advantages of these approaches and exploring whether they can underpin existing assisted reproductive technologies.
卵巢早衰的生物疗法:证据是什么?
卵巢早搏功能不全(POI)是一种影响育龄妇女的多因素疾病。这种情况的特点是在40岁之前卵巢功能丧失,已经确定了几个因素与其发病机制有关。值得注意的是,至少50%的女性在卵巢功能不全后,卵巢中还有剩余的卵泡。人口数据显示,全世界约有3.7%的妇女患有POI和随后的不孕不育。目前,POI相关不孕的治疗涉及卵母细胞捐献。然而,许多患有POI的女性希望怀上自己的卵子。因此,实验性生物疗法,如富血小板血浆(PRP)、外泌体(exo)疗法、体外激活(IVA)、干细胞疗法、微小RNA和线粒体靶向疗法,是专注于激活卵子生成和卵泡生成的实验性治疗策略,通过上调自然生化途径(新卵泡生成)和改善卵巢微环境。这项小型审查旨在确定这些方法的主要优势,并探讨它们是否可以支持现有的辅助生殖技术。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


