Examining the Role of Race in End-of-Life Care in the Intensive Care Unit: A Single-Center Observational Study.
IF 1.1
Q4 HEALTH CARE SCIENCES & SERVICES
Palliative medicine reports
Pub Date : 2023-09-11
eCollection Date: 2023-01-01
DOI:10.1089/pmr.2023.0037
引用次数: 0
Abstract
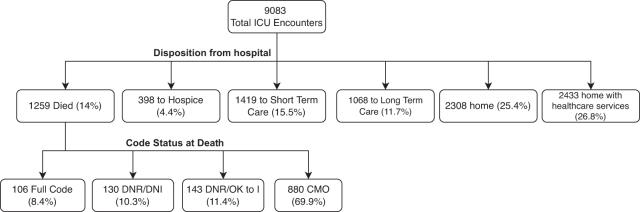
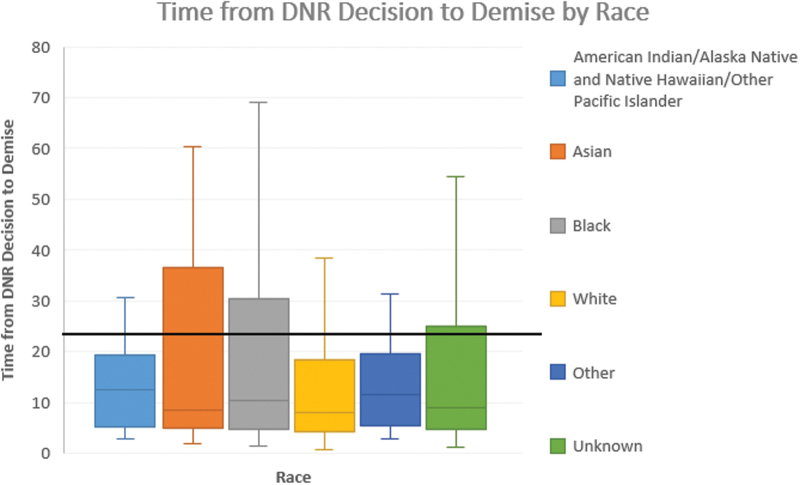
Background: Prior studies have shown variation in the intensity of end-of-life care in intensive care units (ICUs) among patients of different races. Objective: We sought to identify variation in the levels of care at the end of life in the ICU and to assess for any association with race and ethnicity. Design: An observational, retrospective cohort study. Settings: A tertiary care center in Boston, MA. Participants: All critically ill patients admitted to medical and surgical ICUs between June 2019 and December 2020. Exposure: Self-identified race and ethnicity. Main Outcome and Measure: The primary outcome was death. Secondary outcomes included “code status,” markers of intensity of care, consultation by the Palliative care service, and consultation by the Ethics service. Results: A total of 9083 ICU patient encounters were analyzed. One thousand two hundred fifty-nine patients (14%) died in the ICU; the mean age of patients was 64 years (standard deviation 16.8), and 44% of patients were women. A large number of decedents (22.7%) did not have their race identified. These patients had a high rate of interventions at death. Code status varied by race, with more White patients designated as “Comfort Measures Only” (CMO) (74%) whereas more Black patients were designated as “Do Not Resuscitate/Do Not Intubate (DNR/DNI) and DNR/ok to intubate” (12.1% and 15.7%) at the end of life; after adjustment for age and severity of illness, there were no statistical differences by race for the use of the CMO code status. Use of dialysis at the end of life varied by self-identified race. Specifically, Black and Unknown patients were more likely to receive renal replacement therapy, even after adjustment for age and severity of illness (24% and 20%, p = 0.003). Conclusions: Our data describe a gap in identification of race and ethnicity, as well as differences at the end of life in the ICU, especially with respect to code status and certain markers of intensity.
检查种族在重症监护室临终关怀中的作用:一项单中心观察研究。
背景:先前的研究表明,不同种族的患者在重症监护室(ICU)的临终关怀强度存在差异。目的:我们试图确定ICU生命末期护理水平的变化,并评估是否与种族和民族有关。设计:一项观察性、回顾性队列研究。背景:马萨诸塞州波士顿的一家三级护理中心。参与者:2019年6月至2020年12月期间入住医疗和外科重症监护室的所有危重患者。暴露:自我识别的种族和民族。主要结果和衡量标准:主要结果为死亡。次要结果包括“代码状态”、护理强度的标志、姑息治疗服务的咨询和道德服务的咨询。结果:共分析了9083例ICU患者的遭遇。一千二百五十九名患者(14%)死于重症监护室;患者的平均年龄为64岁(标准差16.8),44%的患者为女性。大量死者(22.7%)没有确认其种族。这些患者的干预死亡率很高。代码状态因种族而异,更多的白人患者被指定为“仅限舒适措施”(CMO)(74%),而更多的黑人患者在生命结束时被指定为”不复苏/不插管(DNR/DNI)和DNR/ok插管“(12.1%和15.7%);在对年龄和疾病严重程度进行调整后,CMO代码状态的使用按种族没有统计学差异。生命末期透析的使用因种族而异。具体而言,即使在调整了年龄和疾病严重程度后,黑人和未知患者也更有可能接受肾脏替代治疗(24%和20%,p = 0.003)。结论:我们的数据描述了种族和民族识别方面的差距,以及ICU生命末期的差异,特别是在代码状态和某些强度标记方面。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


