Clinical Features of Patients With Hematological Malignancies Treated at the Palliative Care Unit.
IF 1.1
Q4 HEALTH CARE SCIENCES & SERVICES
Palliative medicine reports
Pub Date : 2023-09-28
eCollection Date: 2023-01-01
DOI:10.1089/pmr.2023.0028
引用次数: 0
Abstract
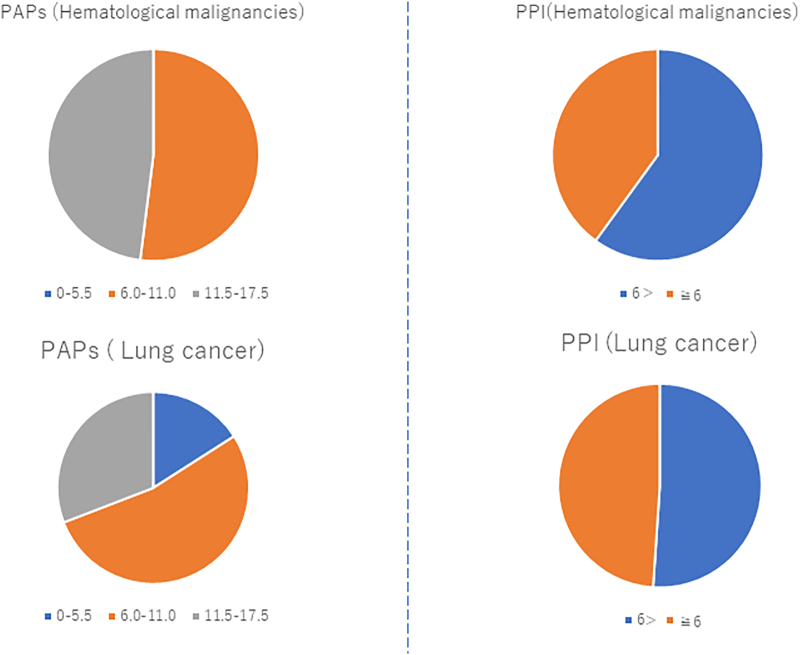
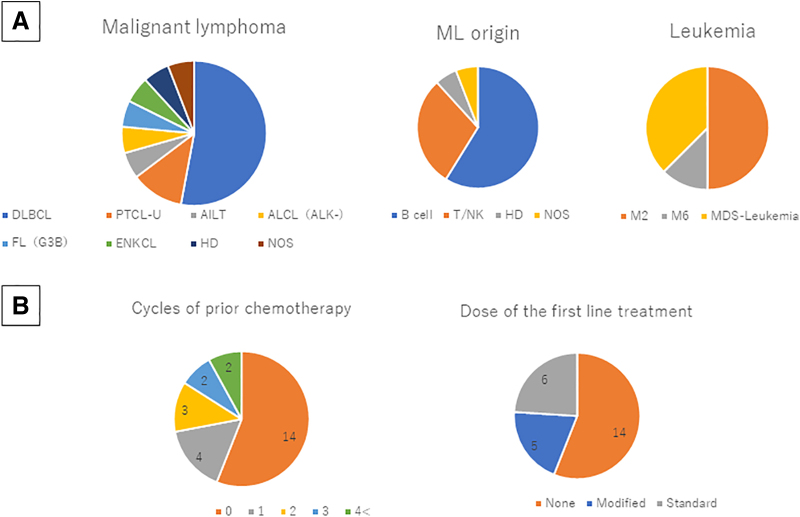
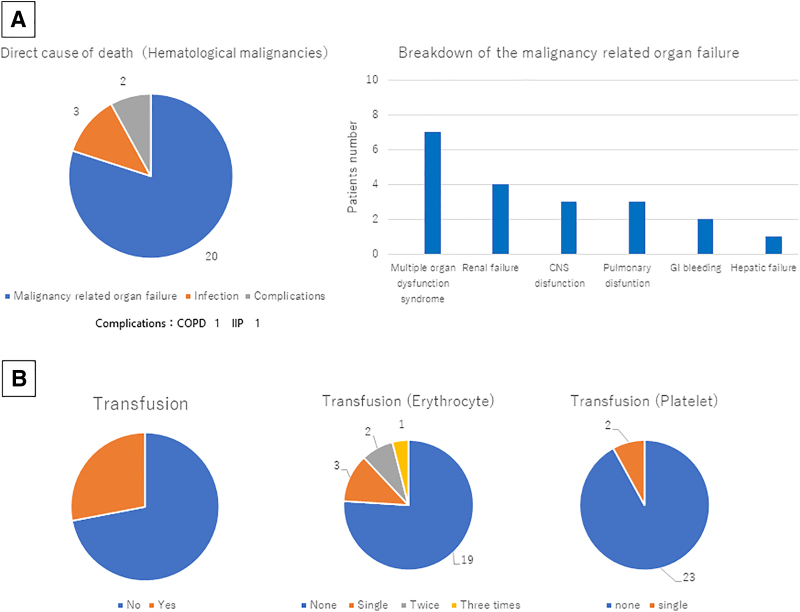
Background: In Japan, the number of patients with aggressive hematological malignancies (PHMs) admitted at the palliative care unit (PCU) in their end-of-life (EOL) stage was fewer than that of patients with solid tumors due to several reasons. The assessment of patient characteristics and the methods of survival prediction among PHMs in the EOL stage are warranted. Objectives: This study aimed to identify the current medical status and the method of survival prediction among PHMs treated at the PCU. Setting/Subjects/Measurements: We retrospectively analyzed the clinical data of 25 PHMs treated at our PCU between January 2017 and December 2020. The association between survival time and the palliative prognostic score (PAP) and palliative prognostic index (PPI) was analyzed. Results: The average age of the PHMs was higher than that of patients with lung cancer as a control. The median survival time of the PHMs was shorter than the control group. Most PHMs could not receive standard chemotherapy, and the most common cause of death was disease-related organ failure. Significant associations were observed between the survival time and each PAP/PPI value in patients with malignant lymphoma, but not in those with leukemia. Conclusion: The PHMs in the PCU had a lower median survival time than the control group. These results were induced by the result of patient selection to avoid treatment-related severe toxicity. The survival prediction using the PAP and PPI was less accurate in patients with leukemia.
在姑息治疗室治疗的血液系统恶性肿瘤患者的临床特征。
背景:在日本,由于几个原因,在姑息治疗室(PCU)接受治疗的晚期恶性血液病患者的数量少于实体瘤患者。EOL阶段PHM的患者特征评估和生存预测方法是有必要的。目的:本研究旨在确定在PCU接受治疗的PHM的当前医疗状况和生存预测方法。设置/受试者/测量:我们回顾性分析了2017年1月至2020年12月期间在PCU治疗的25例PHM的临床数据。分析生存时间与姑息预后评分(PAP)和姑息预后指数(PPI)之间的关系。结果:PHM的平均年龄高于癌症对照组。PHMs的中位生存时间短于对照组。大多数PHM不能接受标准的化疗,最常见的死亡原因是与疾病相关的器官衰竭。恶性淋巴瘤患者的生存时间与每个PAP/PPI值之间存在显著相关性,而白血病患者则没有。结论:PCU的PHMs中位生存时间低于对照组。这些结果是由患者选择的结果引起的,以避免与治疗相关的严重毒性。使用PAP和PPI预测白血病患者的生存率不太准确。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


