Associations of body roundness index with cardiovascular and all-cause mortality: NHANES 2001–2018
IF 2.7
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
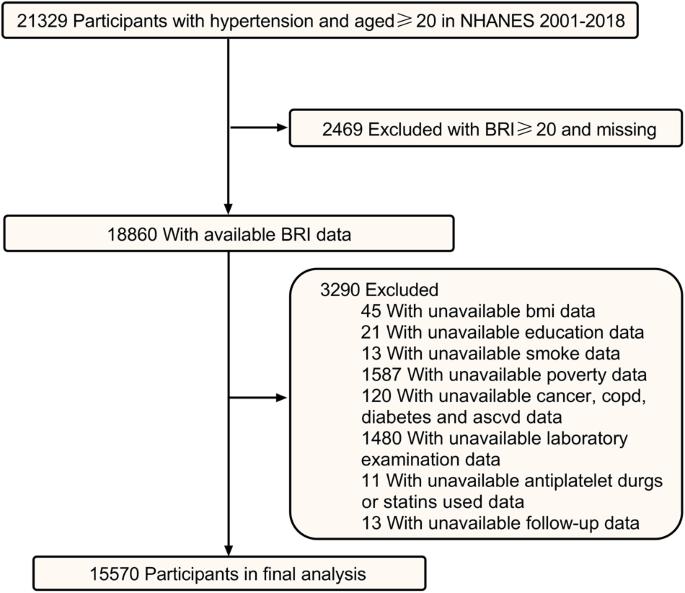
Body roundness index (BRI) was associated with cardiovascular diseases. But the relationship between BRI with cardiovascular disease (CVD) mortality and all-cause mortality remains largely unknown in hypertensive patients. This prospective cohort study included patients with hypertension who participated in the National Health and Nutrition Examination Survey (NHANES) from 2001 through 2018, and aimed to evaluate the association between BRI with CVD mortality and all-cause mortality. A total of 15570 patients were included. Over a median follow-up of 8.0 years (interquartile range, 4.3–12.6 years), 3445 individuals died, including 1166 CVD deaths. Weighted restricted cubic spline regression results showed a nonlinear association between BRI and CVD mortality and all-cause mortality (both P for nonlinear trend <0.001). The weighted multivariate Cox proportional hazards regression showed the hazard ratio (HRs) for CVD mortality were 0.93 (95% CI: 0.84–1.03, P = 0.160) in the low levels of BRI (≤5.9) and 1.11 (95% CI: 1.05–1.19, P < 0.001) in the high levels of BRI (>5.9). Similar associations were observed for all-cause mortality, the HRs were 0.91 (95% CI: 0.87–0.96, P < 0.001) in the low levels of BRI (≤6.3) and 1.09 (95% CI: 1.05–1.13, P < 0.001) in the high levels of BRI (>6.3). This cohort study supported that BRI was nonlinearly associated with CVD mortality and all-cause mortality among patients with hypertension. The thresholds of 5.9 and 6.3 for CVD mortality and all-cause mortality, respectively, may represent intervention targets for lowering the risk of premature death, but this needs to be confirmed in large clinical trials.
身体圆度指数与心血管和全因死亡率的相关性:NHANES 2001-2018。
体圆度指数(BRI)与心血管疾病有关。但是BRI与心血管疾病(CVD)死亡率和高血压患者全因死亡率之间的关系在很大程度上仍然未知。这项前瞻性队列研究包括2001年至2018年参加国家健康和营养检查调查(NHANES)的高血压患者,旨在评估BRI与CVD死亡率和全因死亡率之间的关系。共纳入15570名患者。中位随访8.0年(四分位间距4.3-12.6年),3445人死亡,其中1166人死于心血管疾病。加权限制三次样条回归结果显示,BRI与CVD死亡率和全因死亡率之间存在非线性相关性(非线性趋势均为5.9,P)。全因死亡率也存在类似相关性,HRs为0.91(95%CI:0.87-0.96,P 6.3)。该队列研究支持BRI与高血压患者的CVD死亡率和全因死亡率呈非线性相关。CVD死亡率和全因死亡率的阈值分别为5.9和6.3,可能代表降低过早死亡风险的干预目标,但这需要在大型临床试验中得到证实。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


