Retinal neurodegeneration in eyes with NPDR risk phenotypes: A two-year longitudinal study
Abstract
Introduction
Diabetic retinopathy (DR) is both a microangiopathy and a neurodegenerative disease. However, the connections between both changes are not well known.
Purpose
To characterise the longitudinal retinal ganglion cell layer + inner plexiform layer (GCL + IPL) changes and their association with microvascular changes in type-2 diabetes (T2D) patients with nonproliferative diabetic retinopathy (NPDR).
Methods
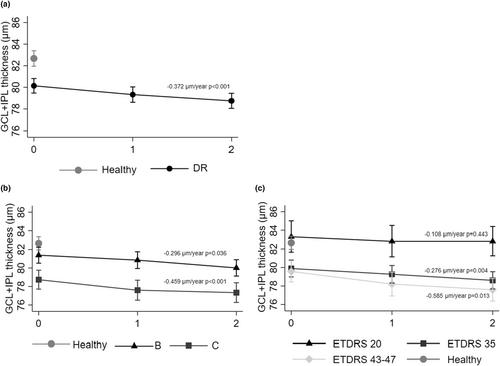
This two-year prospective study (CORDIS, NCT03696810) included 122 T2D individuals with NPDR identified as risk phenotypes B and C, which present a more rapid progression. Phenotype C was identified by decreased VD ≥ 2SD in healthy controls, and phenotype B, identified by subclinical macular oedema with only minimal vascular closure. The GCL + IPL thickness, vessel density, perfusion density and area of intercapillary spaces (AIS) were assessed by optical coherence tomography (OCT) and OCT angiography (OCTA). Linear mixed effects models were employed to evaluate the retinal GCL + IPL progression and its associations.
Results
Regarding GCL + IPL thickness, T2D individuals presented on average 80.1 ± 7.49 μm, statistically significantly lower than the healthy control group, 82.5 ± 5.71 (p = 0.022), with only phenotype C differing significantly from controls (p = 0.006). GCL + IPL thickness steadily decreased during the two-year period in both risk phenotypes, with an annual decline rate of −0.372 μm/year (p < 0.001). Indeed, phenotype C showed a higher rate of progression (−0.459 μm/year, p < 0.001) when compared to phenotype B (−0.296 μm/year, p = 0.036). Eyes with ETDRS grade 20 showed GCL + IPL thickness values comparable to those of healthy control group (83.3 ± 5.80 and 82.7 ± 5.50 μm, respectively, p = 0.880), whereas there was a progressive decrease in GCL + IPL thickness in ETDRS grades 35 and 43–47 associated with the increase in severity of the retinopathy (−0.276 μm/year, p = 0.004; −0.585 μm/year, p = 0.013, respectively). Furthermore, the study showed statistically significant associations between the progressive thinning of GCL + IPL and the progressive increase in retinal capillary non-perfusion, with particular relevance for AIS (p < 0.001).
Conclusions
Our findings showed that, in eyes with NPDR and at risk for progression, retinal neurodegeneration occurs at different rates in different risk phenotypes, and it is associated with retinal microvascular non-perfusion.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


