Critical care, maternal and neonatal outcomes of pregnant women with COVID-19 admitted to eight intensive care units during the wildtype, alpha and delta waves of the pandemic across the North West of England—a retrospective review
Abstract
Introduction
Few studies have described obstetric and critical care outcomes in pregnant women with COVID-19 needing intensive care unit (ICU) admission.
Material and methods
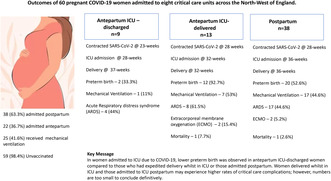
Obstetric and critical care outcomes of COVID-19 women admitted to eight ICUs from April 1, 2020 to September 15, 2021, in the North West of England were retrospectively analyzed. Women admitted to ICU were assigned to three groups: antepartum women discharged from ICU prior to delivery (antepartum ICU-discharged group), antepartum women who had expedited delivery (antepartum ICU-delivered group) and a postpartum group. Our aims were to describe maternal characteristics and assess how delivery influenced the obstetric and critical care outcomes in these women.
Results
During the study period, 615 women tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), of whom 62 (10.1%) needed ICU admission due to symptomatic COVID-19. Pregnancy loss (3.2%) was recorded in two women. Detailed obstetric and critical outcomes from 60 women are reported. Nine antepartum women (15%) admitted to ICU were discharged and continued their pregnancy, 13 antepartum women (21.7%) had expedited delivery by cesarean birth after ICU admission and 38 (63.3%) women were admitted to ICU during the postpartum period. Antepartum ICU-discharged women contracted the SARS-CoV-2 at an earlier median gestational age (23 weeks; p = 0.0003) and needed ICU admission at an earlier median gestational age (28 weeks, p = 0.03) compared with antepartum ICU-delivered (28 and 32 weeks) and postpartum women (35.5 and 36 weeks). Antepartum ICU-discharged women had the lowest rate of mechanical ventilation receipt (11.1%) compared with antepartum ICU-delivered women (52.3%) and postpartum women (44.3%) but the difference was not statistically significant (p = 0.13). No significant differences were observed in the frequency and severity of critical care complications in the antepartum ICU-discharged, antepartum-ICU delivered and postpartum women.
Conclusions
Of the women admitted to ICU antepartum, 40% were discharged while remaining pregnant and 60% had expedited delivery. Antepartum women who were discharged from ICU without giving birth may receive lower rates of mechanical ventilation than those who delivered in ICU or admitted postpartum; however, further studies are needed to confirm or refute this association.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


