Analysis of clinicopathological characteristics and prognostic factors of early-stage human epidermal growth factor receptor 2 (HER2)-low breast cancer: Compared with HER2-0 breast cancer
Abstract
Purpose
To investigate the clinicopathological characteristics and prognostic factors of early-stage breast cancer (EBC) with human epidermal growth factor receptor 2 (HER2)-low expression.
Methods
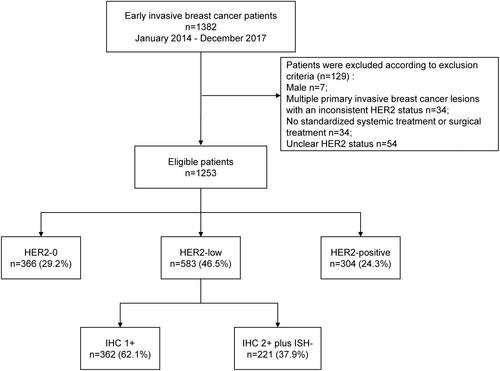
The clinicopathological data and follow-up information of EBC patients with HER2-low and HER2-0 expression treated at the Breast Disease Center of Peking University First Hospital from January 2014 to December 2017 were analyzed. The prognosis between HER2-low and HER2-0 expression groups and with different hormone receptor (HR) expression were compared by statistics. Meanwhile, the expression of Ki67, androgen receptor (AR), TOPIIa, P53, PTEN, and CK5/6 were also analyzed with the HER2-low expression and prognosis.
Results
Retrospectively analyzed 1253 cases of EBC, including 583 (46.5%) cases of HER2-low breast cancer (BC) and 366 (29.2%) HER2-0 BC cases. Among the HER2-low BC patients, 487 (83.5%) were HR-positive, while 96 (16.5%) were HR-negative. Among the HER2-0 BC patients, 265 (72.4%) were HR-positive, while 101 (27.6%) were HR-negative. Median follow-up time was 53 months. The 5-year disease-free survival of HER2-low BC patients was 90.2% (95% confidence interval [CI]: 87.2–93.1), and the 5-year overall survival was 95.4% (95% CI: 93.3–97.6). Cox regression analysis showed that T stage, lymphovascular invasion, and/or perineural invasion were prognostic factors of HER2-low BC patients. However, the 5-year disease-free survival and overall survival of patients in the HER2-low and HER2-0 groups were not significantly different in all patients, but a tendency of better prognosis in HER2-low group was seen in HR-negative tumors.
Conclusion
HER2-low EBC patients accounted for 46.5% of the patient population. T stage, lymphovascular invasion, and/or perineural invasion were factors affecting the prognosis of BC patients with low HER2 expression. No significant difference in prognosis was noted between HER2-low and HER2-0 EBC patients. But in HR-negative tumors, a tendency of better prognosis was seen in HER2-low versus HER2-0.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


