Spontaneous pneumomediastinum; Time for a consensus.
IF 1.2
Q3 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Cardiovascular and Thoracic Research
Pub Date : 2022-01-01
Epub Date: 2022-08-30
DOI:10.34172/jcvtr.2022.26
引用次数: 107
Abstract
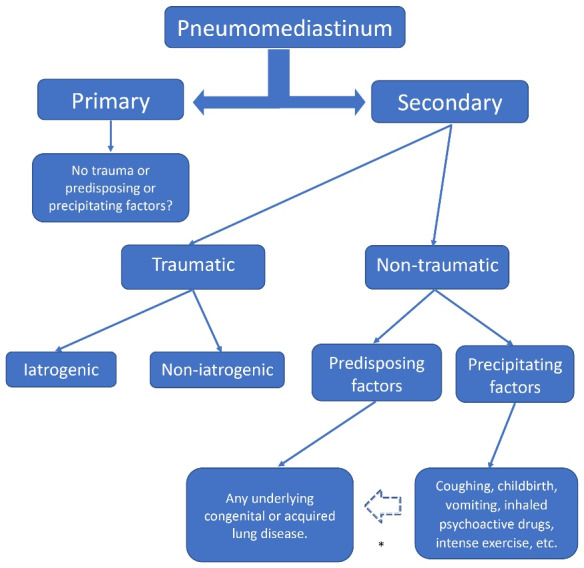
Dear Editor, Considering the article published by Hülya Dirol and Hakan Keskin: Risk factors for mediastinitis and mortality in Pneumomediastinum,1 I would like to respectfully give my opinion on the so-called spontaneous pneumomediastinum. We agree in dividing pneumomediastinum into primary and secondary, but we consider that the primary is the truly spontaneous or idiopathic, terms that should be omitted and called primary. This pneumomediastinum cannot have any predisposing or precipitating factor. The secondary, can in turn be traumatic and non-traumatic, and the latter is where the predisposing and precipitating factors influence (Figure 1). According to current literature, any pneumomediastinum that is not traumatic is “spontaneous”, but it happens that the group called spontaneous is the one with the greatest triggering cause. This creates confusion and causes conceptual difficulty. We believe that the classification should evolve towards greater accuracy. For us, if a PM has a predisposing factor that compromises the pulmonary structure whether congenital, hereditary, or genetic (bronchiectasis, cystic fibrosis, surfactant alterations, etc.) or acquired (asthma, COPD, interstitial lung disease, COVID-19, etc.), it cannot be spontaneous because there is an underlying predisposing disease. Similarly, the pneumomediastinum that occurs due to a precipitating factor (coughing, labor, intense exercise, use of inhaled drugs, mechanical ventilation, etc.) in a healthy subject or with an underlying lung disease cannot be
自发的纵隔气肿;是时候达成共识了。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Cardiovascular and Thoracic Research
CARDIAC & CARDIOVASCULAR SYSTEMS-
CiteScore
2.00
自引率
0.00%
发文量
22
审稿时长
7 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


