Unusual Case of Iatrogenic Inadvertent Diversion of the Inferior Vena Cava Into the Left Atrium in a Patient With Atrial Septal Defect: Diagnosed by the Intraoperative Transesophageal Echocardiography.
Q2 Medicine
引用次数: 0
Abstract
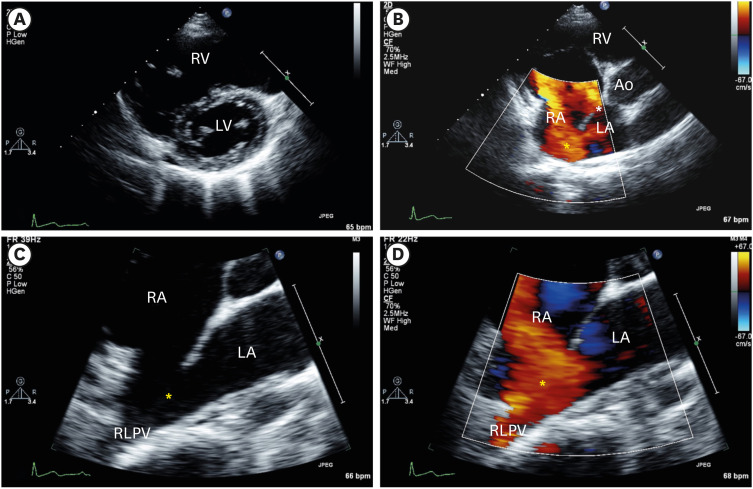
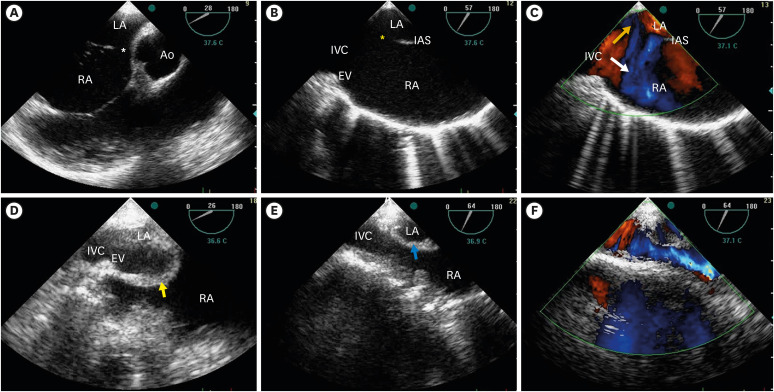
https://e-jcvi.org An 18-year-old girl was referred for an atrial septal defect (ASD) closure. Transthoracic echocardiography (TTE) revealed a small secundum ASD near the aortic root and another large posteroinferior-lying ASD (Figure 1). The measured Qp:Qs was 2.5:1. Intraoperative transesophageal echocardiography (TEE) also demonstrated findings similar to TTE (Figure 2A-C). Under standard cardiopulmonary bypass (CPB), the surgeon closed 2 defects using pericardial patches. After weaning from the first CPB, the systemic oxygen saturation suddenly decreased to 82%. Emergently performed intraoperative TEE revealed that the lower margin of patch closure was incorporated into the Eustachian valve, and the blood flow was diverted from the inferior vena cava (IVC) into the left atrium (LA) (Figure 2D, Movie 1). On the second CPB, the surgeon repositioned the patch and reconnected the IVC to the right atrium (Figure 2E and F, Movies 2 and 3). The second CPB was weaned, and the systemic oxygen saturation was 100%.
术中经食管超声心动图诊断房间隔缺损患者下腔静脉不小心转入左心房的罕见病例。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Cardiovascular Imaging
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
3.40
自引率
0.00%
发文量
42
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


