Review of the current use of global lung function initiative norms for spirometry (GLI-2012) and static lung volumes (GLI-2021) in Great Arab Maghreb (GAM) countries and steps required to improve their utilization.
IF 16.4
1区 化学
Q1 CHEMISTRY, MULTIDISCIPLINARY
引用次数: 2
Abstract
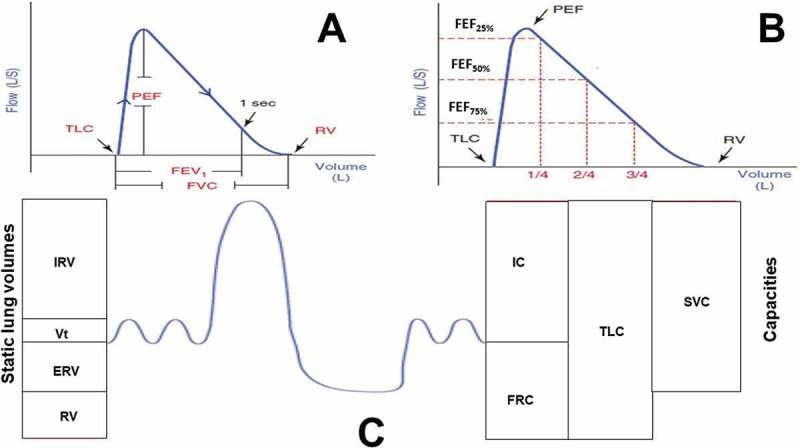
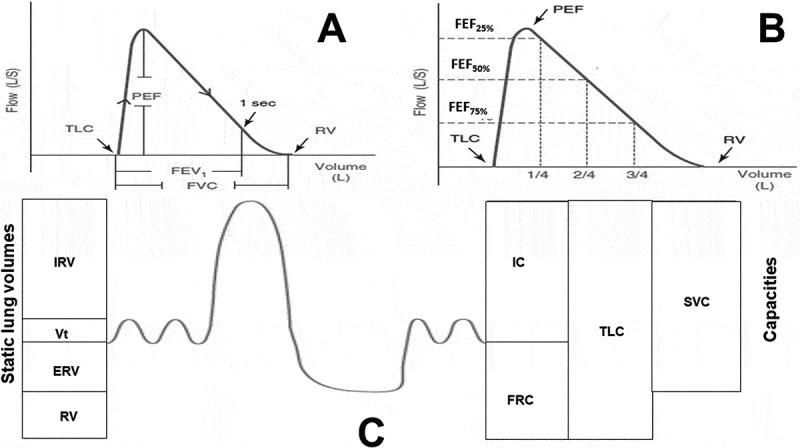
The respiratory functional defects can be evaluated by some tests exploring the ventilatory mechanics, such as spirometry and plethysmography, which determine airflows, dynamic lung volumes, and static lung volumes (SLVs) [1–4] (Figure 1). Indeed, the decrease in some spirometric [e.g.; ratio between the forced expiratory volume in the first second and the forced vital capacity (FEV1/FVC)] or SLV [e.g.; total lung capacity (TLC)] parameters allow to diagnose, respectively, obstructive ventilatory (OVD) and restrictive ventilatory (RVD) defects, and to assess their severities [1–4]. Inversely, the increase of other parameters [e.g.; residual volume (RV), functional residual capacity (FRC)] retains the diagnosis of lung-hyperinflation [1–3]. According to some scholarly societies [1–5], the interpretation of the spirometric/SLV parameters requires a series of four steps [6]. The first is a comparison of the parameters measured/calculated with these of reference predicted using norms (i.e.; reference equations) [1,2]. These norms are derived from tests carried out within a representative sample of the general population (i.e.; “healthy/normal’ subjects), having similar anthropometric, ethnic, socio-economic and environmental characteristics as the patient tested [1–3]. According to the American thoracic society (ATS), a ‘healthy’ person is defined as one in whom there is: i) no presence of acute and no past chronic condition of the pulmonary system; ii) no major pulmonary condition in past medical history; iii) no systemic condition which may impact the pulmonary system and general state of well-being; iv) no history of upper respiratory tract infection during three weeks prior to exploration, and v) normal body composition taking into account ethnic group, vi) no more than incidental smoking experience (in children), vii) gestational age at least 37 weeks, and birthweight at least 2.5 kg (in infants), viii) no history of other than transient respiratory problems during the neonatal period (in infants), and ix) lifelong nonsmokers, or no more than incidental smoking experience (in adults) [7]. Some authors have suggested more stringent criteria for defining ‘health’ [8]. In the absence of specific intra-individual norms, the interpretation of spirometric/SLV parameters often encounters difficulties [6]. Indeed, trustworthy interpretation of spirometric/plethysmographic results relies on the availability of appropriate norms to help differentiate between ‘health’ and ‘disease’ and to evaluate the severity and nature of any ventilatory defect [4,5,9]. Among the five countries of the GAM (namely Tunisia, Algeria, Libya, Morocco, and Mauritania), only Mauritania has not established any spirometric/SLVs norms. Tunisia, Libya, Algeria, and Morocco has some spirometric and/or SLVs norms [10–21]. The second step is a comparison of the determined parameter’ value with the distinctive thresholds of the main ventilatory defects (VDs) noted during chronic diseases [e.g.; OVD, RVD, mixed VD, non-specific VD, lung-hyperinflation) [1,2,4]. In this context, norms are useful for classifying a spirometric/SLV parameter as decreased, normal or increased based on fixed thresholds (e.g.; 0.70, 70% or 80%) [22], or more better on the 95% confidence interval (e.g.; lower limit of normal (LLN), upper limit of normal (ULN)) [1,2]. It is worth noting that the method based on a fixed threshold has major limitations [23–25]. First, it is documented that the FEV1/FVC ratio declines with increasing age and height, even in healthy lifelong nonsmokers, in whom the LLN drops below a ratio of
审查大阿拉伯马格里布(GAM)国家目前使用全球肺功能倡议肺活量测定规范(glii -2012)和静态肺容量规范(glii -2021)的情况,以及改善其使用所需的步骤。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Accounts of Chemical Research
化学-化学综合
CiteScore
31.40
自引率
1.10%
发文量
312
审稿时长
2 months
期刊介绍:
Accounts of Chemical Research presents short, concise and critical articles offering easy-to-read overviews of basic research and applications in all areas of chemistry and biochemistry. These short reviews focus on research from the author’s own laboratory and are designed to teach the reader about a research project. In addition, Accounts of Chemical Research publishes commentaries that give an informed opinion on a current research problem. Special Issues online are devoted to a single topic of unusual activity and significance.
Accounts of Chemical Research replaces the traditional article abstract with an article "Conspectus." These entries synopsize the research affording the reader a closer look at the content and significance of an article. Through this provision of a more detailed description of the article contents, the Conspectus enhances the article's discoverability by search engines and the exposure for the research.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


