Considering Psychosocial Factors When Investigating Blood Pressure in Patients with Short Sleep Duration: A Propensity Score Matched Analysis.
IF 1.9
4区 医学
Q3 PERIPHERAL VASCULAR DISEASE
International Journal of Hypertension
Pub Date : 2021-11-30
eCollection Date: 2021-01-01
DOI:10.1155/2021/7028942
引用次数: 1
Abstract
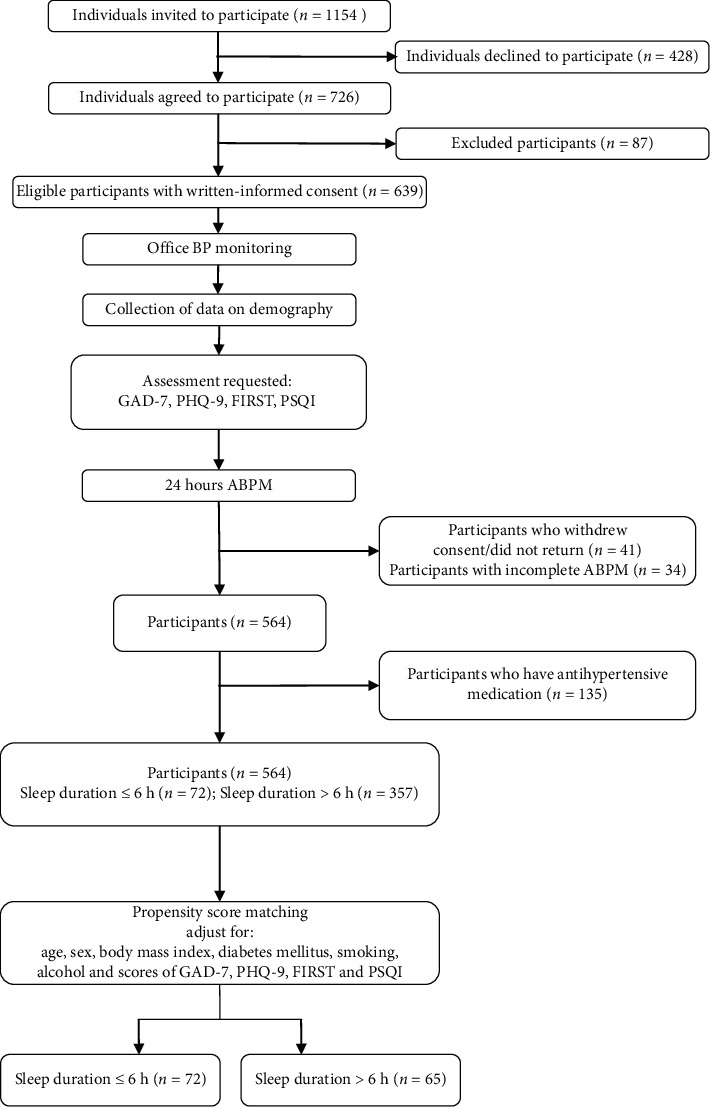
Few studies have considered psychosocial characteristics when investigating the associations between sleep duration and blood pressure (BP). In this study, we took propensity score matching (PSM) to adjust for psychosocial characteristics when comparing BP between individuals with short sleep duration and those with normal sleep duration. A total of 429 participants were included. 72 participants with sleep duration ≤6 h and 65 participants with sleep duration >6 h were matched after PSM. We compared office BP, 24-hour BP, and prevalence of hypertension in the populations before and after PSM, respectively. In the unmatched population, participants with sleep duration ≤6 h were observed with higher office diastolic BP (DBP) and 24-h systolic BP (SBP)/DBP (all P < 0.05). In the matched populations, the differences between the two groups (sleep duration ≤6 h vs. sleep duration >6 h) in office DBP (88.4 ± 10.9 vs. 82.5 ± 11.1 mm Hg; P=0.002), 24-h SBP (134.7 ± 12.0 vs. 129.3 ± 11.6 mm Hg; P=0.009), and 24-h DBP (83.4 ± 9.9 vs. 78.1 ± 10.1 mm Hg; P=0.002) become more significant. Participants with sleep duration ≤6 h only show higher prevalence of hypertension based on 24-h BP data, while analysis after PSM further revealed that these with sleep duration ≤6 h presented about 20% higher prevalence of elevated BP up to office diagnosed hypertension threshold. Therefore, psychosocial characteristics accompanied with short sleep duration should be fully valued in individuals at risks for elevated BP. This trial is registered with NCT03866226.
在调查睡眠时间短患者的血压时考虑心理社会因素:倾向得分匹配分析。
在调查睡眠时间和血压之间的关系时,很少有研究考虑到心理社会特征。在本研究中,我们采用倾向得分匹配(PSM)来调整心理社会特征,以比较睡眠时间短和睡眠时间正常的个体的血压。共纳入429名参与者。睡眠时间≤6 h的受试者72名,睡眠时间>6 h的受试者65名。我们分别比较了PSM前后人群的办公室血压、24小时血压和高血压患病率。在未匹配的人群中,睡眠时间≤6 h的参与者的办公室舒张压(DBP)和24小时收缩压(SBP)/DBP均较高(P < 0.05)。在匹配人群中,两组(睡眠时间≤6 h vs睡眠时间>6 h)办公室DBP差异(88.4±10.9 vs 82.5±11.1 mm Hg;P = 0.002), 24小时SBP(134.7±12.0和129.3±11.6毫米汞柱;P = 0.009), 24小时菲律宾(83.4±9.9和78.1±10.1毫米汞柱;P=0.002)变得更加显著。根据24小时血压数据,睡眠时间≤6小时的参与者仅显示出较高的高血压患病率,而PSM后的分析进一步显示,睡眠时间≤6小时的参与者血压升高至办公室诊断的高血压阈值的患病率约高出20%。因此,对于有血压升高风险的个体,应充分重视伴随睡眠时间短的社会心理特征。本试验注册号为NCT03866226。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
International Journal of Hypertension
Medicine-Internal Medicine
CiteScore
4.00
自引率
5.30%
发文量
45
期刊介绍:
International Journal of Hypertension is a peer-reviewed, Open Access journal that provides a forum for clinicians and basic scientists interested in blood pressure regulation and pathophysiology, as well as treatment and prevention of hypertension. The journal publishes original research articles, review articles, and clinical studies on the etiology and risk factors of hypertension, with a special focus on vascular biology, epidemiology, pediatric hypertension, and hypertensive nephropathy.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


