Malayan Pit Viper Envenomation and Treatment in Thailand.
IF 4.6
Q2 MATERIALS SCIENCE, BIOMATERIALS
ACS Applied Bio Materials
Pub Date : 2021-11-30
eCollection Date: 2021-01-01
DOI:10.2147/TCRM.S337199
引用次数: 7
Abstract
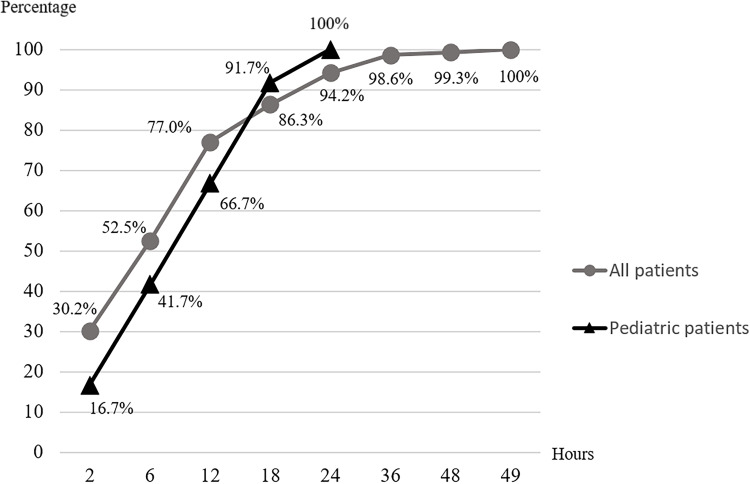
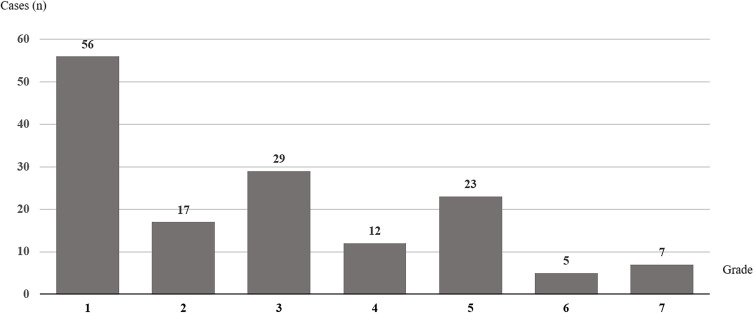
Introduction The Malayan pit viper (MPV; Calloselasma rhodostoma) is a hematotoxic snake found in all regions of Thailand and many countries in Southeast Asia. Treatment of MPV envenomation varies among facilities due to their capabilities. Materials and Methods This study was a retrospective review of patients with MPV envenomation who were reported to the Ramathibodi Poison Center from 1 July 2016 to 30 June 2018. Results Of the 167 patients (median age, 40.5 years; range, 1.3–87.0 years) bitten by an MPV, the most common bite site was the foot (29.3%). Most patients reached the hospital within 1 hour of being bitten. One-hundred fifty-six patients (93.4%) had local effects from envenomation; 17 patients (10.2%) had severe local complications including necrotizing fasciitis (3.0%) and compartment syndrome (7.2%). Systemic effects such as hemorrhage and abnormal hemostasis occurred in 147 patients (88.0%). Additional effects included abnormal venous clotting time in 123 patients (73.7%), unclotted 20-minute whole blood clotting time in 57 patients (34.1%), low platelet counts (<50,000/µL) in 29 patients (17.4%), prolonged international normalized ratio (>1.2) in 51 patients (30.5%), and systemic bleeding in 14 patients (8.4%). The median onset of bleeding disorder was 6 hours. Monitoring for 24, 48, and 49 hours after bite enabled detection of systemic effects in 94.2%, 99.3%, and 100.0%, respectively. Three hundred fifteen courses of antivenin were administered to 144 patients (86.2%). All the patients who received antivenin recovered from bleeding disorder. Only 7.0% of antivenin doses were administered without Thai Red Cross indications. Allergic reactions from antivenin occurred in 34.7% of the 144 patients. One hundred thirty patients (77.8%) received antibiotics, and 32 patients (19.2%) required surgical management, including debridement and fasciotomy. Conclusion MPV envenomation results in local and systemic effects. Most systemic effects were abnormal clotting test results. Most patients reported onset of bleeding disorder within 48 hours.

泰国马来亚蝮蛇的中毒和治疗。
简介:马来亚蝮蛇(MPV;是一种血毒蛇,在泰国所有地区和东南亚许多国家都有发现。MPV污染的处理因设施的能力而异。材料和方法:本研究是对2016年7月1日至2018年6月30日向Ramathibodi毒物中心报告的MPV中毒患者的回顾性研究。结果:167例患者(中位年龄40.5岁;年龄在1.3 ~ 87.0岁之间),最常见的咬伤部位是足部(29.3%)。大多数患者在被咬后一小时内被送往医院。156例(93.4%)患者出现局部中毒反应;17例(10.2%)有严重的局部并发症,包括坏死性筋膜炎(3.0%)和筋膜室综合征(7.2%)。147例(88.0%)患者出现出血、止血异常等全身反应。其他影响包括123例(73.7%)患者静脉凝血时间异常,57例(34.1%)患者未凝血的20分钟全血凝血时间,51例(30.5%)患者血小板计数低(1.2),14例(8.4%)患者全身出血。出血性疾病的中位发病时间为6小时。咬伤后24小时、48小时和49小时的监测结果分别为94.2%、99.3%和100.0%。144例患者(86.2%)接受315个疗程的抗蛇毒血清治疗。所有接受抗蛇毒血清治疗的患者均从出血性疾病中恢复。只有7.0%的抗蛇毒血清剂量没有泰国红十字会的适应症。144例患者中抗蛇毒血清过敏反应发生率为34.7%。130例患者(77.8%)接受抗生素治疗,32例患者(19.2%)需要手术治疗,包括清创和筋膜切开术。结论:MPV中毒可引起局部和全身影响。大多数全身效应是异常的凝血试验结果。大多数患者报告在48小时内出现出血性疾病。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


