How prevalent and severe is addiction on GABAmimetic drugs in an elderly German general hospital population? Focus on gabapentinoids, benzodiazepines, and z-hypnotic drugs
Abstract
Objective
Gabapentinoids (GPT) are reported to be increasingly misused by opioid- and polydrug-users, but the addictive potential of GPT outside of these populations remains understudied. Investigations comparing GPT abuse and dependence liability to that of other commonly prescribed Central Nervous System-acting medications are therefore warranted. We provide a comparison of GPT-abuse/dependence to that of other GABAmimetics within an elderly population.
Design
DSM-IV-TR-based data (previously prospectively collected by SKID-I-interview) from a random sample of elderly patients admitted to a metropolitan German general hospital were reviewed. The prevalence and severity of GPT, benzodiazepine (BDZ), and z-hypnotic drug (ZD)-abuse and -dependence were compared, stratified also by mono-substance (no concurrent current or previous substance use) and de novo-substance (first)-abuse and -dependence states.
Results
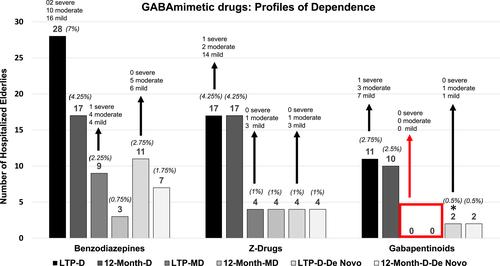
Among 400 patients (75 ± 6.4 years old; 63% females), neither current nor past abuse of BDZ, ZD or GPT, nor other illicit substances was observed. Dependence upon BDZ, ZD or GPT was observed among 55 (13.75%) individuals. The related lifetime/12-month prevalence-rates were: dependence condition (BDZ: 7%/2.45%; ZD: 4.25%/4.25%; GPT: 2.75/2.5%); mono-dependence condition (BDZ: 2.25%/0.75%; ZD: 1%/1%, GPT: 0%/0%); de novo-dependence condition (BDZ: 2.75%/1.75%; ZD: 1%/1%, GPT: 0.5%/0.5%). Opioid analgesic-dependence (N = 43/400) was significantly more frequently linked with BDZ than with GPT (p < 0.01) [Correction added on 29 December 2021, after first online publication: In the sentence ‘Opioid analgesic-dependence…’, the term ‘and ZD’ has been deleted]. For all three GABAmimetic classes, most mono- and de novo-dependence states were mild-to-moderate and lasted 2–6 years (median).
Conclusion
GABAmimetic-dependence was usually mixed with other substance-dependences. Every third to fourth instance of BDZ- or ZD-dependence was a mono-dependence condition, while a pure GPT-dependence was absent in this elderly (and illicit substance-naïve) population.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


