Urinary albumin-to-creatinine ratio and the risk of first stroke in Chinese hypertensive patients treated with angiotensin-converting enzyme inhibitors
IF 4.3
2区 医学
Q1 PERIPHERAL VASCULAR DISEASE
引用次数: 3
Abstract
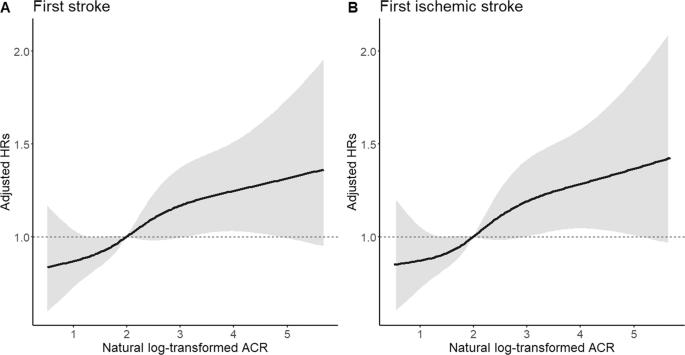
We aimed to evaluate the relationship of the albumin-to-creatinine ratio (ACR) with the risk of first stroke and examine possible effect modifiers in hypertensive patients. A total of 11,632 hypertensive participants with urinary ACR measurements and without a history of stroke from the China Stroke Primary Prevention Trial (CSPPT) were included in this analysis. The primary outcome was first stroke. Over a median follow-up of 4.4 years, 728 first strokes were identified, of which 633 were ischemic, 89 were hemorrhagic, and 6 were uncertain types. Overall, there was a significant positive association between natural log-transformed ACR and the risk of first stroke (HR, 1.11; 95% CI: 1.03–1.20) and first ischemic stroke (HR, 1.12; 95% CI: 1.03–1.22). Consistently, participants with ACR ≥ 10 mg/g had a significantly higher risk of first stroke (HR, 1.26; 95% CI: 1.06–1.50) and first ischemic stroke (HR, 1.33; 95% CI: 1.10–1.59) than those with ACR < 10 mg/g. Moreover, the association of ACR with first stroke was significantly stronger in participants with higher total homocysteine (tHcy) levels (<10 versus ≥ 10 μmol/L; P for interaction = 0.044). However, there was no significant association between ACR and first hemorrhagic stroke (per natural log [ACR] increment: HR, 1.02; 95% CI: 0.82–1.27). In summary, hypertensive patients with ACR ≥ 10 mg/g had a significantly increased risk of first stroke or first ischemic stroke. This positive association was more pronounced among participants with higher tHcy levels.
尿白蛋白-肌酐比值与接受血管紧张素转换酶抑制剂治疗的中国高血压患者首次中风的风险
我们旨在评估白蛋白肌酐比值(ACR)与高血压患者首次脑卒中风险的关系,并研究可能的影响因素。本次分析共纳入了中国脑卒中一级预防试验(CSPPT)中 11,632 名测量过尿液 ACR 且无脑卒中病史的高血压患者。主要结果是首次中风。在中位随访 4.4 年期间,共发现 728 例首次脑卒中,其中 633 例为缺血性脑卒中,89 例为出血性脑卒中,6 例为不确定类型的脑卒中。总体而言,自然对数转换后的 ACR 与首次中风风险(HR,1.11;95% CI:1.03-1.20)和首次缺血性中风风险(HR,1.12;95% CI:1.03-1.22)呈显著正相关。同样,与 ACR < 10 mg/g 的参与者相比,ACR ≥ 10 mg/g 的参与者发生首次中风(HR,1.26;95% CI:1.06-1.50)和首次缺血性中风(HR,1.33;95% CI:1.10-1.59)的风险明显更高。此外,总同型半胱氨酸(tHcy)水平较高者(<10 与 ≥ 10 μmol/L;交互作用 P = 0.044)的 ACR 与首次中风的相关性明显更强。然而,ACR 与首次出血性卒中之间无明显关联(每自然对数 [ACR] 增量:HR,1.02;95% CI:0.82-1.27)。总之,ACR ≥ 10 mg/g 的高血压患者首次中风或首次缺血性中风的风险明显增加。这种正相关在 tHcy 水平较高的参与者中更为明显。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Hypertension Research
医学-外周血管病
CiteScore
7.40
自引率
16.70%
发文量
249
审稿时长
3-8 weeks
期刊介绍:
Hypertension Research is the official publication of the Japanese Society of Hypertension. The journal publishes papers reporting original clinical and experimental research that contribute to the advancement of knowledge in the field of hypertension and related cardiovascular diseases. The journal publishes Review Articles, Articles, Correspondence and Comments.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


