A Clinical Monitoring Program of COVID-19 Outpatients: A Prospective Cohort Study.
The Canadian journal of infectious diseases & medical microbiology = Journal canadien des maladies infectieuses et de la microbiologie medicale
Pub Date : 2021-07-20
eCollection Date: 2021-01-01
DOI:10.1155/2021/6644570
引用次数: 1
Abstract
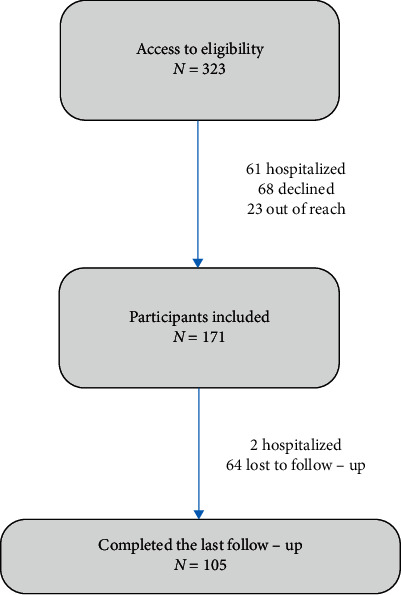
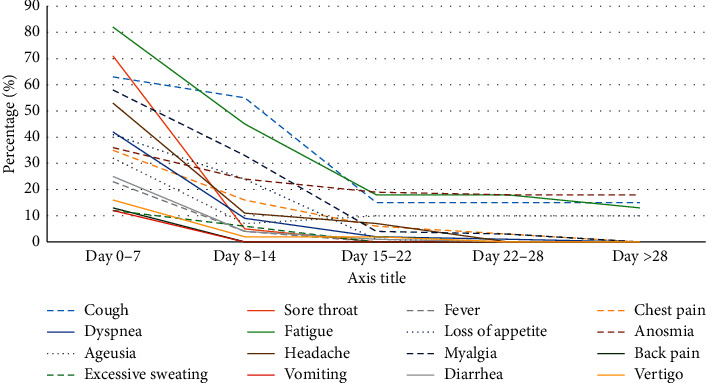
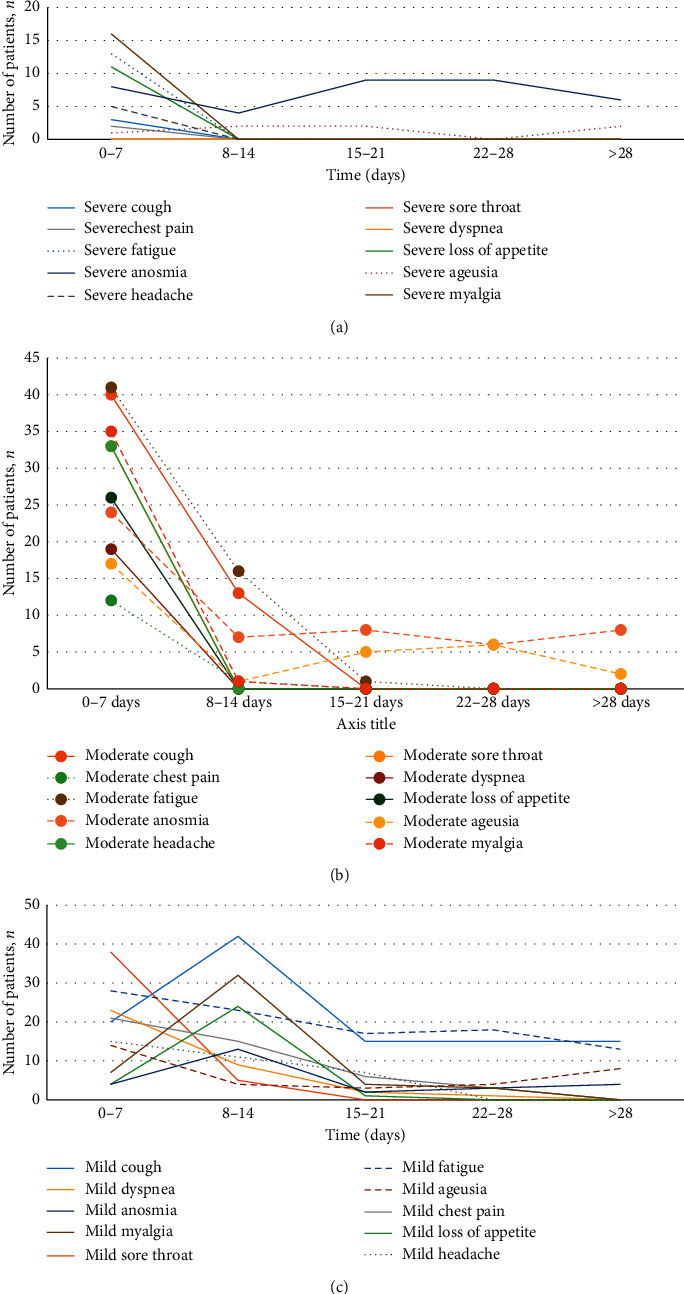
Purpose Coronavirus disease 2019 (COVID-19) has been associated with a high rate of mortality and morbidity. While a high portion of COVID-19 patients have mild symptoms, a limited number of clinical trials have evaluated the clinical course of this large group of patients. This study was designed to investigate the demographics and clinical characteristics and comorbidity of nonhospitalized COVID-19 patients. Methods This prospective, observational cohort study was performed on nonhospitalized adult patients (≥18 years) with COVID-19. Pharmacotherapy service was responsible for patients' assessment for up to 1 month. Demographic characteristics, the onset of symptoms, severity, duration, laboratory data, and hospitalization rate were evaluated by a pharmacist-based monitoring program. Results From 323 patients who had been referred to the emergency department, 105 individuals were recruited between April 26 and August 2, 2020. Most of the patients were female (66.7%) with a mean age of 39.39 years (SD: ± 15.82). The mean time of the symptom onset was 5.6 days (SD: ±1.79). The majority of patients suffered from fatigue (78.1%), sore throat (67.6%), cough (60%), and myalgia (55.2%). C-reactive protein, white blood cell, lymphocyte, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and hemoglobin levels were recovered significantly during the first two weeks (P < 0.001). Hydroxychloroquine, naproxen, diphenhydramine, azithromycin, and vitamin D3 were the most common medications administered (98%, 96%, 94%, 68%, and 57%, respectively). Forty patients were not symptom-free after the one-month follow-up, and 8 patients (7.6%) were required to revisit without the need for hospitalization. Anosmia (18.1%) and fatigue (17.1%) were the most common persisted symptoms. There were no significant differences between symptom-free and symptomatic patients. Conclusion Mild COVID-19 patients had a wide variety of symptoms and could be symptomatic even one month after the onset of symptoms. The pharmacist-based monitoring system can contribute beneficially to patients through the evaluation of symptoms, reduction of unnecessary visits, and provision of updated information to patients concerning the status of their illness.
COVID-19门诊患者临床监测项目:一项前瞻性队列研究
目的:2019冠状病毒病(COVID-19)与高死亡率和发病率相关。虽然很大一部分COVID-19患者症状轻微,但有限数量的临床试验评估了这一大群患者的临床病程。本研究旨在调查非住院COVID-19患者的人口统计学特征、临床特征和合并症。方法:这项前瞻性、观察性队列研究对未住院的成年COVID-19患者(≥18岁)进行了研究。药物治疗服务负责患者长达1个月的评估。通过以药剂师为基础的监测程序评估人口统计学特征、症状发作、严重程度、持续时间、实验室数据和住院率。结果:从323名转诊到急诊科的患者中,在2020年4月26日至8月2日期间招募了105人。患者以女性居多(66.7%),平均年龄39.39岁(SD:±15.82)。平均出现症状时间为5.6 d (SD:±1.79)。大多数患者表现为疲劳(78.1%)、喉咙痛(67.6%)、咳嗽(60%)和肌痛(55.2%)。c反应蛋白、白细胞、淋巴细胞、中性粒细胞与淋巴细胞比值、血小板与淋巴细胞比值和血红蛋白水平在前两周显著恢复(P < 0.001)。羟氯喹、萘普生、苯海拉明、阿奇霉素和维生素D3是最常用的药物(分别为98%、96%、94%、68%和57%)。40例患者随访1个月后症状仍未消除,8例(7.6%)患者无需住院,需再次就诊。嗅觉丧失(18.1%)和疲劳(17.1%)是最常见的持续症状。无症状患者与有症状患者之间无显著差异。结论:轻症COVID-19患者症状多样,甚至在出现症状一个月后仍可能出现症状。以药剂师为基础的监测系统可以通过评估症状、减少不必要的就诊和向患者提供有关其疾病状况的最新信息,从而对患者有益。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
自引率
0.00%
发文量
0

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


