Immunological response to COVID-19 and its role as a predisposing factor in invasive aspergillosis.
Q3 Medicine
引用次数: 6
Abstract
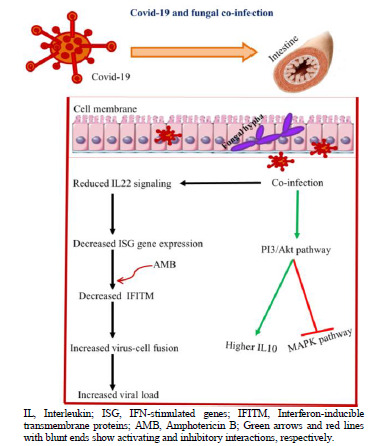
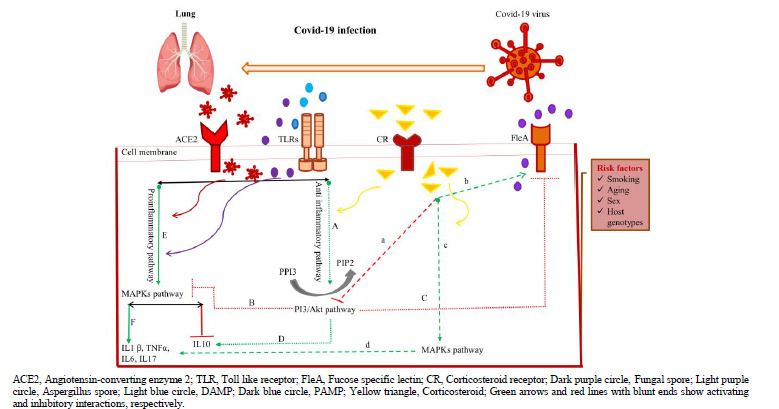
The world is involved with a pandemic coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2. The clinical manifestations of reported COVID-19-associated pulmonary impairments range from asymptomatic infections to a pneumonia-induced acute respiratory distress syndrome that requires mechanical ventilation. Fungal superinfections complicating the clinical course remain underexplored. Angiotensin-converting enzyme 2, the receptor for COVID-19 that is mainly expressed in airway epithelia and lung parenchyma, is considered an important regulator of innate immunity. With regard to the viral-cell interaction, imbalanced immune regulation between protective and altered responses caused by the exacerbation of inflammatory responses should be considered a major contributor to secondary pulmonary aspergillosis. In addition, the complex inherited factors, age-related changes, and lifestyle may also affect immune responses. The complication and persistence of invasive aspergillosis have been well described in patients with severe influenza or COVID-19. However, there is a scarcity of information about the immunological mechanisms predisposing patients with COVID-19 to fungal co-infections. Therefore, this study was conducted to investigate the aforementioned domain.
对COVID-19的免疫反应及其作为侵袭性曲霉病易感因素的作用
世界正面临由严重急性呼吸综合征冠状病毒2引起的2019年大流行性冠状病毒疾病(新冠肺炎)。报告的COVID-19相关肺损伤的临床表现从无症状感染到需要机械通气的肺炎诱导的急性呼吸窘迫综合征。使临床过程复杂化的真菌重叠感染仍然没有得到充分的研究。血管紧张素转化酶2是新冠肺炎的受体,主要表达于气道上皮和肺实质,被认为是先天免疫的重要调节因子。关于病毒与细胞的相互作用,炎症反应恶化引起的保护性反应和改变性反应之间的免疫调节失衡应被认为是继发性肺曲霉菌病的主要原因。此外,复杂的遗传因素、与年龄相关的变化和生活方式也可能影响免疫反应。侵袭性曲霉菌病的并发症和持续性在严重流感或新冠肺炎患者中得到了很好的描述。然而,关于新冠肺炎患者易患真菌合并感染的免疫机制的信息很少。因此,本研究旨在研究上述领域。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Current Medical Mycology
Medicine-Infectious Diseases
CiteScore
2.10
自引率
0.00%
发文量
16
审稿时长
4 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


