Noninvasive Neurally Adjusted Ventilator Assist Ventilation in the Postoperative Period Produces Better Patient-Ventilator Synchrony but Not Comfort.
IF 2
Q3 RESPIRATORY SYSTEM
引用次数: 2
Abstract
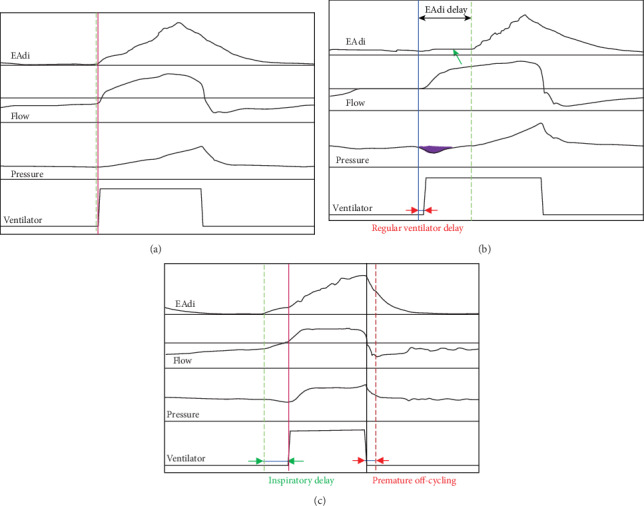
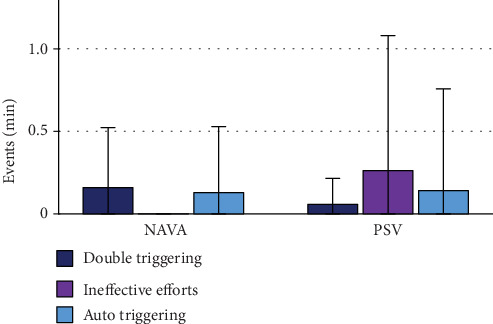
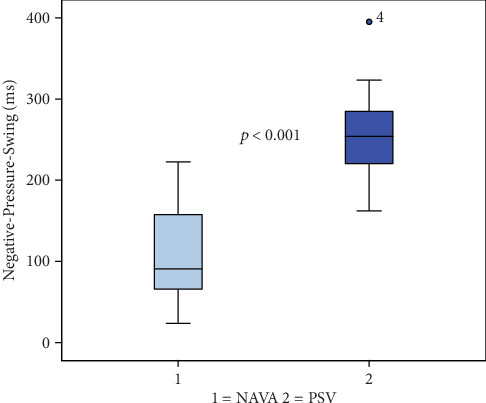
Background Noninvasive neurally adjusted ventilatory assist (NAVA) has been shown to improve patient-ventilator interaction in many settings. There is still scarce data with regard to postoperative patients indicated for noninvasive ventilation (NIV) which this study elates. The purpose of this trial was to evaluate postoperative patients for synchrony and comfort in noninvasive pressure support ventilation (NIV-PSV) vs. NIV-NAVA. Methods Twenty-two subjects received either NIV-NAVA or NIV-PSV in an object-blind, prospective, randomized, crossover fashion (observational trial). We evaluated blood gases and ventilator tracings throughout as well as comfort of ventilation at the end of each ventilation phase. Results There was an effective reduction in ventilator delays (p < 0.001) and negative pressure duration in NIV-NAVA as compared to NIV-PSV (p < 0.001). Although we used optimized settings in NIV-PSV, explaining the overall low incidence of asynchrony, NIV-NAVA led to reductions in the NeuroSync-index (p < 0.001) and all types of asynchrony except for double triggering that was significantly more frequent in NIV-NAVA vs. NIV-PSV (p = 0.02); ineffective efforts were reduced to zero by use of NIV-NAVA. In our population of previously lung-healthy subjects, we did not find differences in blood gases and patient comfort between the two modes. Conclusion In the postoperative setting, NIV-NAVA is well suitable for use and effective in reducing asynchronies as well as a surrogate for work of breathing. Although increased synchrony was not transferred into an increased comfort, there was an advantage with regard to patient-ventilator interaction. The trial was registered at the German clinical Trials Register (DRKS no.: DRKS00005408).
术后无创神经调节呼吸机辅助通气改善患者-呼吸机同步但不舒适。
背景:在许多情况下,无创神经调节通气辅助(NAVA)已被证明可以改善患者与呼吸机的相互作用。关于术后患者需要无创通气(NIV)的数据仍然很少,这是本研究的成果。本试验的目的是评估术后患者在无创压力支持通气(NIV-PSV)与NIV-NAVA中的同步性和舒适性。方法:22名受试者采用对象盲、前瞻性、随机、交叉方式(观察性试验)接受NIV-NAVA或NIV-PSV治疗。我们评估了整个过程中的血气和呼吸机追踪以及每个通气阶段结束时的通气舒适度。结果:与NIV-PSV相比,NIV-NAVA有效减少了呼吸机延迟(p < 0.001)和负压持续时间(p < 0.001)。虽然我们在NIV-PSV中使用了优化的设置,解释了整体异步发生率较低,但NIV-NAVA导致神经同步指数降低(p < 0.001)和所有类型的异步,除了NIV-NAVA比NIV-PSV更频繁的双重触发(p = 0.02);使用NIV-NAVA将无效工作减少到零。在我们先前肺部健康的受试者人群中,我们没有发现两种模式之间血气和患者舒适度的差异。结论:术后使用NIV-NAVA可有效减少不同步,是呼吸工作的替代。虽然增加的同步性并没有转化为增加的舒适度,但在患者与呼吸机的相互作用方面有一个优势。该试验已在德国临床试验注册(DRKS号:: DRKS00005408)。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


