Low-fluoroscopy atrial fibrillation ablation with contact force and ultrasound technologies: a learning curve.
IF 2.7
Q2 MEDICINE, GENERAL & INTERNAL
Pragmatic and Observational Research
Pub Date : 2019-01-10
eCollection Date: 2019-01-01
DOI:10.2147/POR.S181220
引用次数: 7
Abstract
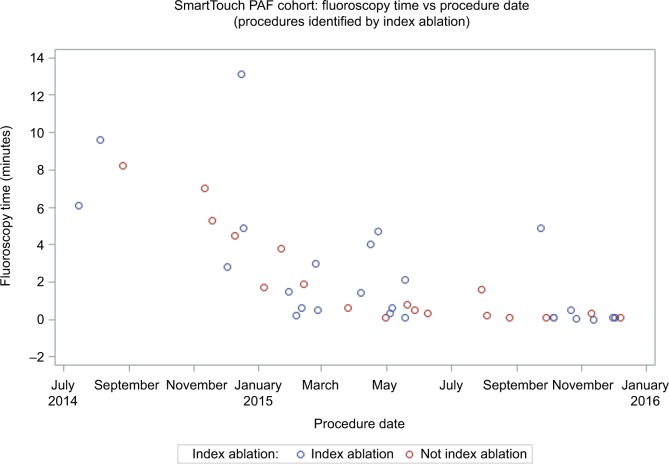
Background Fluoroscopy exposure during catheter ablation is a health hazard to patients and operators. This study presents the results of implementing a low-fluoroscopy workflow using modern contact force (CF) technologies in paroxysmal atrial fibrillation (PAF) ablation. Methods A fluoroscopy reduction workflow was implemented and subsequent catheter ablations for PAF were evaluated. After vascular access with ultrasound guidance, a THERMOCOOL SMARTTOUCH® Catheter (ST) was advanced into the right atrium. The decapolar catheter was placed without fluoroscopy. A double-transseptal puncture was performed under intracardiac echocardiography guidance. ST and mapping catheters were advanced into the left atrium. A left atrial map was created, and pulmonary vein (PV) isolation was confirmed via entrance and exit block before and after the administration of isoproterenol or adenosine. Results Forty-three patients underwent PAF ablation with fluoroscopy reduction workflow (mean age: 66±9 years; 70% male), performed by five operators. Acute success rate (PV isolation) was 96.5% of PVs. One case of pericardial effusion, not requiring intervention, was the only acute complication. Mean procedure time was 217±42 minutes. Mean fluoroscopy time was 2.3±3.0 minutes, with 97.7% of patients having < 10 minutes and 86.0% having < 5 minutes. A significant downward trend over time was observed, suggesting a rapid learning curve for fluoroscopy reduction. Freedom from any atrial arrhythmias without reablation was 80.0% after a mean follow-up of 12±3 months. Conclusion Low fluoroscopy time is achievable with CF technologies after a short learning curve, without compromising patient safety or effectiveness.
低透视心房颤动消融与接触力和超声技术:一个学习曲线。
背景:导管消融过程中的透视暴露对患者和手术者都是一种健康危害。本研究介绍了在阵发性心房颤动(PAF)消融中使用现代接触力(CF)技术实现低透视工作流程的结果。方法:实施透视复位工作流程,并对PAF的后续导管消融进行评估。在超声引导下进入血管后,将THERMOCOOL SMARTTOUCH®导管(ST)推进至右心房。在没有透视的情况下放置脱斜导管。在超声心动图引导下行双隔穿刺。ST和定位导管进入左心房。在异丙肾上腺素或腺苷给药前后,绘制左心房图,通过进出阻断确认肺静脉(PV)隔离。结果:43例患者行PAF消融加透视复位流程(平均年龄66±9岁;70%为男性),由5名操作人员执行。急性成功率(PV分离)为96.5%。1例心包积液是唯一的急性并发症,无需干预。平均手术时间217±42分钟。平均透视时间为2.3±3.0分钟,97.7%的患者< 10分钟,86.0%的患者< 5分钟。随着时间的推移,观察到明显的下降趋势,表明透视复位的快速学习曲线。平均随访12±3个月,无房性心律失常复发率为80.0%。结论:CF技术在短时间学习曲线后可以实现低透视时间,而不会影响患者的安全性或有效性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Pragmatic and Observational Research
MEDICINE, GENERAL & INTERNAL-
自引率
0.00%
发文量
11
期刊介绍:
Pragmatic and Observational Research is an international, peer-reviewed, open-access journal that publishes data from studies designed to closely reflect medical interventions in real-world clinical practice, providing insights beyond classical randomized controlled trials (RCTs). While RCTs maximize internal validity for cause-and-effect relationships, they often represent only specific patient groups. This journal aims to complement such studies by providing data that better mirrors real-world patients and the usage of medicines, thus informing guidelines and enhancing the applicability of research findings across diverse patient populations encountered in everyday clinical practice.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


