Metformin decreases progerin expression and alleviates pathological defects of Hutchinson–Gilford progeria syndrome cells
IF 4.1
Q2 GERIATRICS & GERONTOLOGY
引用次数: 38
Abstract
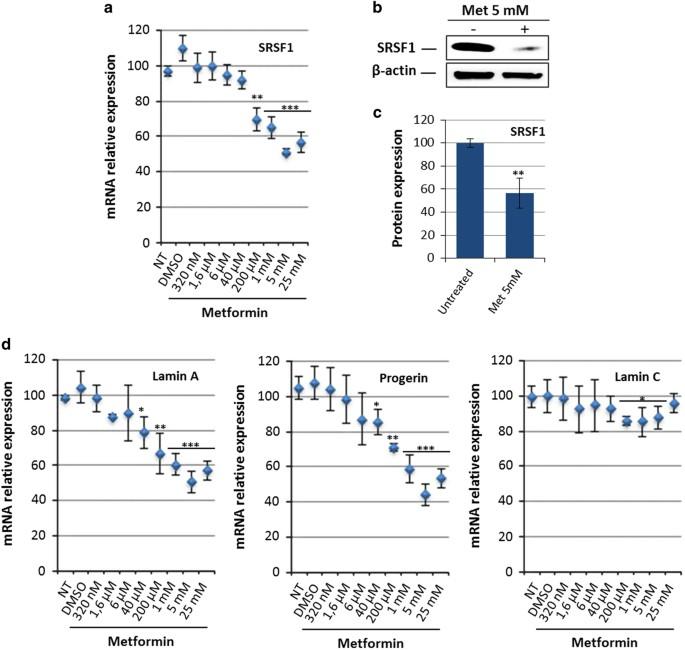
Hutchinson–Gilford progeria syndrome (HGPS) is a rare genetic disorder that causes systemic accelerated aging in children. This syndrome is due to a mutation in the LMNA gene that leads to the production of a truncated and toxic form of lamin A called progerin. Because the balance between the A-type lamins is controlled by the RNA-binding protein SRSF1, we have hypothesized that its inhibition may have therapeutic effects for HGPS. For this purpose, we evaluated the antidiabetic drug metformin and demonstrated that 48 h treatment with 5 mmol/l metformin decreases SRSF1 and progerin expression in mesenchymal stem cells derived from HGPS induced pluripotent stem cells (HGPS MSCs). The effect of metformin on progerin was then confirmed in several in vitro models of HGPS, i.e., human primary HGPS fibroblasts, LmnaG609G/G609G mouse fibroblasts and healthy MSCs previously treated with a PMO (phosphorodiamidate morpholino oligonucleotide) that induces progerin. This was accompanied by an improvement in two in vitro phenotypes associated with the disease: nuclear shape abnormalities and premature osteoblastic differentiation of HGPS MSCs. Overall, these results suggest a novel approach towards therapeutics for HGPS that can be added to the currently assayed treatments that target other molecular defects associated with the disease. A diabetes drug with a proven track record in the clinic may also offer an alternative treatment for a rare ''premature aging'' disorder. A genetic mutation in patients with Hutchinson-Gilford progeria syndrome (HGPS) produces a defective protein called progerin, which causes children to develop skeletal, cardiovascular and other symptoms normally seen in the elderly. Researchers led by Xavier Nissan at I-Stem in France have demonstrated that metformin triggers a biochemical ''switch'' that causes cells to decrease their production of progerin, and instead generate an alternative, non-toxic protein. Relative to untreated cells, metformin-treated cells were less prone to develop structural abnormalities or undergo premature maturation. Importantly, doctors have used metformin for over 20 years, suggesting that such a treatment approach should be safe for HGPS patients.
二甲双胍可减少早老素的表达,缓解 Hutchinson-Gilford 早老综合征细胞的病理缺陷
哈钦森-吉尔福德早衰综合症(HGPS)是一种罕见的遗传性疾病,会导致儿童全身加速衰老。这种综合征是由于 LMNA 基因突变导致产生一种被称为早衰素的截短的有毒片层蛋白 A。由于 A 型片层蛋白之间的平衡是由 RNA 结合蛋白 SRSF1 控制的,因此我们假设抑制 SRSF1 可能对 HGPS 有治疗作用。为此,我们评估了抗糖尿病药物二甲双胍,结果表明,用5毫摩尔/升二甲双胍处理48小时后,SRSF1和早衰素在HGPS诱导多能干细胞(HGPS间充质干细胞)间充质干细胞中的表达会减少。二甲双胍对早衰素的影响随后在几种 HGPS 体外模型中得到了证实,这些模型包括人类原代 HGPS 成纤维细胞、LmnaG609G/G609G 小鼠成纤维细胞和先前用诱导早衰素的 PMO(磷酰二胺吗啉寡核苷酸)处理过的健康间充质干细胞。与此同时,与该疾病相关的两种体外表型也得到了改善:HGPS 间充质干细胞的核形状异常和过早成骨分化。总之,这些结果为治疗 HGPS 提出了一种新的方法,可以添加到目前针对与该疾病相关的其他分子缺陷的治疗方法中。一种已在临床上证明有效的糖尿病药物也可能为罕见的 "早衰 "疾病提供另一种治疗方法。哈钦森-吉尔福特早衰综合征(HGPS)患者的基因突变会产生一种名为早老素的缺陷蛋白,这种蛋白会导致儿童出现骨骼、心血管和其他通常在老年人身上出现的症状。法国 I-Stem 公司的泽维尔-尼桑领导的研究人员证明,二甲双胍能触发一种生化 "开关",使细胞减少早老素的产生,转而生成一种替代性的无毒蛋白质。与未经处理的细胞相比,二甲双胍处理过的细胞不易出现结构异常或过早成熟。重要的是,医生使用二甲双胍已有20多年的历史,这表明这种治疗方法对HGPS患者是安全的。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


