Macular Evaluation wıth Spectral Domain Type Optic Coherence Tomography in Eyes with Acute Nonarteritic Ischemic Optic Neuropathy at the Presentation Visit.
The Open Ophthalmology Journal
Pub Date : 2017-01-31
eCollection Date: 2017-01-01
DOI:10.2174/1874364101711010017
引用次数: 3
Abstract
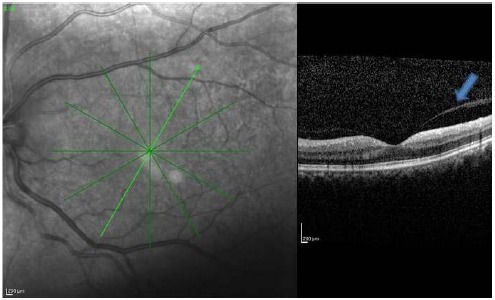
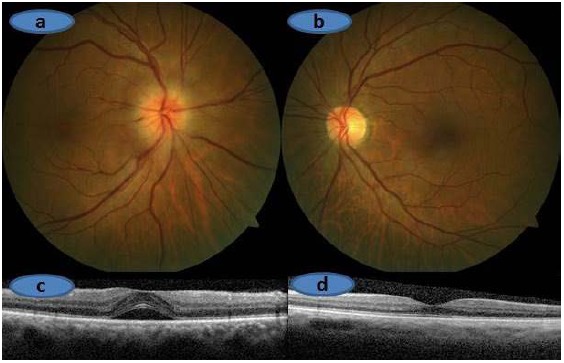
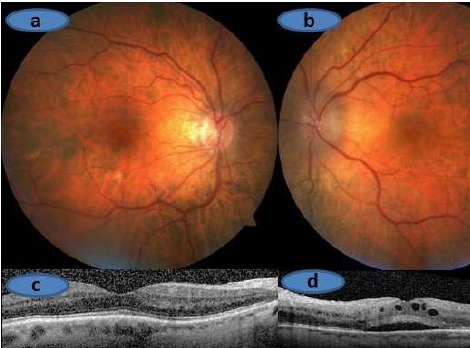
Purpose: To evaluate the macula with spectral domain type optic coherence tomography (OCT) in eyes with acute nonarteritic anterior ischemic optic neuropathy (NAION) at the presentation visit. Methods: Medical charts of the 133 patients who received the diagnosis of acute NAION between January 2008 and July 2014 at the Neuro-ophthalmology unit of Dokuz Eylul University were reviewed retrospectively. Sixtythree patients within 30 days of symptom onset with available baseline spectral domain type macular OCT were included in this study. Clinical and macular characteristics of the affected eye were assessed and compared to the fellow eyes. Results: Sixty-three eyes of 63 patients comprised the study group. Twenty one study eyes (33.3%) had normal posterior pole, 22 (34.9%) some evidence of subretinal fluid, 10 (15.8%) vitreomacular adhesion, five (7%) age-related macular degeneration related changes, four (6%) epiretinal membrane and one (1%) previous grid laser scars. On the other hand, 41 of 63 the fellow eyes (65%) had normal posterior pole, ten (15.8%), vitreomacular adhesion, seven (10.7%), age-related macular degeneration related changes, three (4%) epiretinal membrane and two (3%) other type of changes. OCT scan passing through the fovea exhibited 10 or more hyperreflective dots in 10 (15%) of the study eyes whereas two of the fellow eyes (3.2%) had 10 or more hyperreflective dots. Conclusion: Macular OCT can be a part of the routine neuroophthalmologic examination in patients with acute NAION not only to show the NAION related changes such as the subretinal fluid accumulation but also to identify the other coexistent macular abnormalities.
黄斑评估wıth频谱域型光学相干断层扫描在急性非动脉性缺血性视神经病变的介绍访问。
目的:应用光谱域型光学相干断层扫描(OCT)评价急性非动脉性前缺血性视神经病变(NAION)的黄斑表现。方法:回顾性分析2008年1月至2014年7月在Dokuz Eylul大学神经眼科就诊的133例急性NAION患者的病历。本研究纳入63例症状出现30天内可用基线谱域型黄斑OCT的患者。评估受影响眼睛的临床和黄斑特征,并与其他眼睛进行比较。结果:63例患者共63只眼组成研究组。21只眼(33.3%)后极正常,22只眼(34.9%)有视网膜下积液,10只眼(15.8%)有玻璃体黄斑粘连,5只眼(7%)有老年性黄斑变性相关改变,4只眼(6%)有视网膜前膜,1只眼(1%)有既往网格激光疤痕。另一方面,63只眼中41只(65%)后极正常,10只(15.8%),玻璃体黄斑粘连,7只(10.7%),年龄相关性黄斑变性相关改变,3只(4%)视网膜前膜,2只(3%)其他类型的改变。通过中央凹的OCT扫描显示10只眼睛(15%)有10个或更多的高反射点,而另外两只眼睛(3.2%)有10个或更多的高反射点。结论:黄斑OCT可以作为急性NAION患者常规神经眼科检查的一部分,不仅可以显示NAION相关的改变,如视网膜下积液,还可以发现其他并发的黄斑异常。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


