Benefits of future clean air policies in Europe: Proposed analyses of the mortality impacts of PM2.5 and NO2.
IF 3.8
Q2 ENVIRONMENTAL SCIENCES
Environmental Epidemiology
Pub Date : 2022-08-31
eCollection Date: 2022-10-01
DOI:10.1097/EE9.0000000000000221
引用次数: 6
Abstract
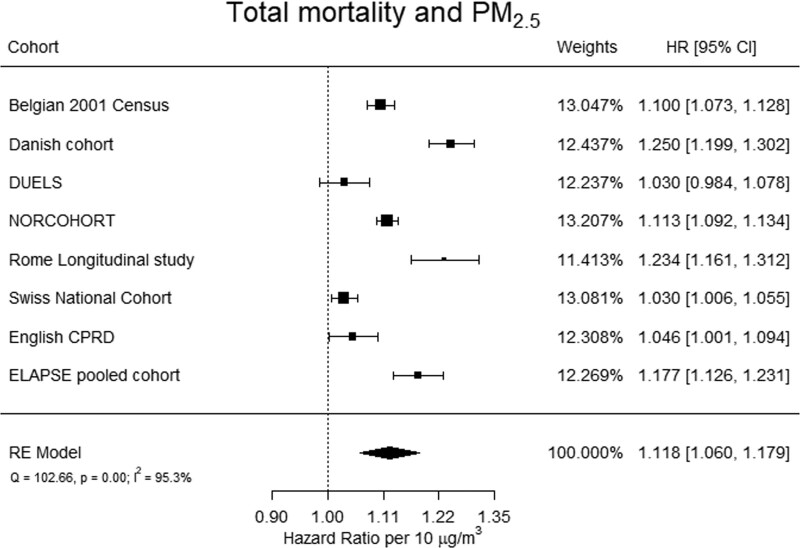
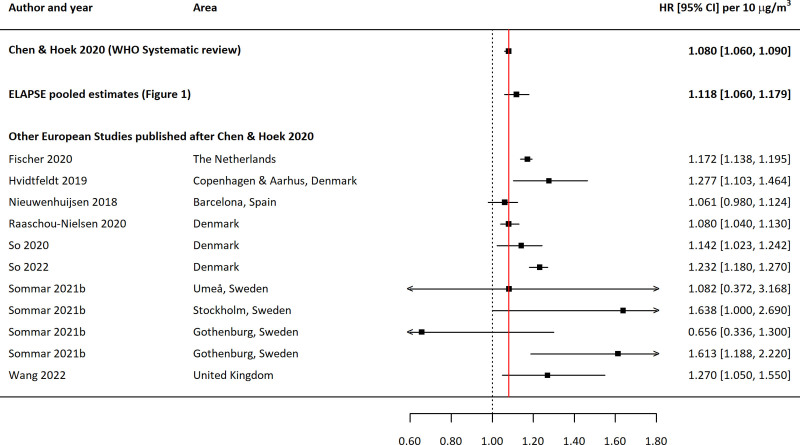
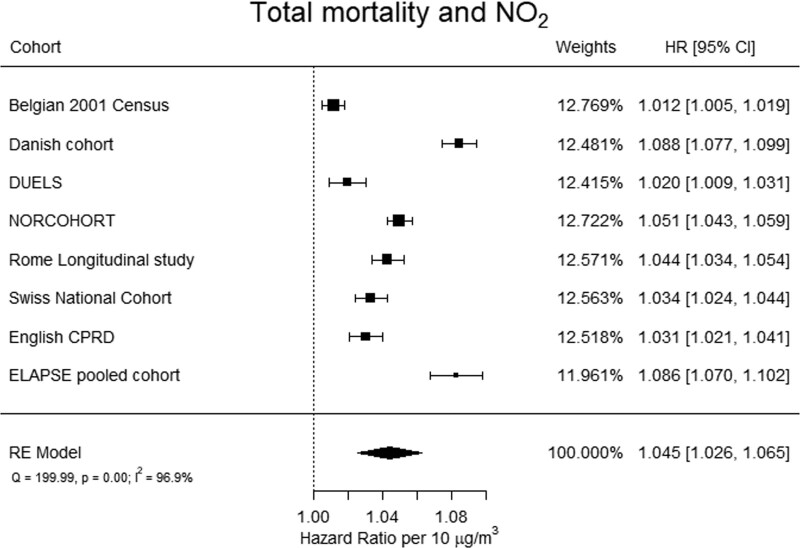
Health impact assessments (HIA) and cost-benefit analyses (CBA) play a major role in the ongoing revision of the European Union Ambient Air Quality Directive (EU AAQD). HIAs quantify the public health impacts of the air pollution levels a population is exposed to. CBAs quantify the economic costs of achieving lower air pollution levels and the (monetized) benefits for public health that result from these lower air pollution levels. In this commentary, we consider the recent body of evidence on the effects of long-term exposure to fine particulate matter (PM2.5) and nitrogen dioxide (NO2) on total mortality from natural causes and present the rationale for conducting additional analyses within the framework of the HIA conducted for the revision of the EU AAQD, based on the recently published European “Effects of Low-Level Air Pollution: A Study in Europe” (ELAPSE) study. The air pollution-related burden (presented as impact on mortality from natural causes) for Europe has been estimated since 2014 in the annual “Air Quality in Europe” reports published by the European Environment Agency (EEA). EEA in their HIA has used relative risk estimates from meta-analyses by Hoek and colleagues1 in 2013, based on evidence published before January 2013: 1.06 (1.04, 1.08) for PM2.5 and 1.05 (1.03, 1.08) for NO2, both per 10 μg/m 3. The EEA, in its latest HIA for 2019, assumed no threshold for PM2.5, and a threshold of 20 μg/m3 for NO2, and estimated 307,000 and 40,400 premature deaths in the EU27 associated with PM2.5 and NO2, respectively. 2 In support of the recent development of the 2021 World Health Organization (WHO) Air Quality Guidelines, new systematic reviews of the evidence of effects of air pollutants on mortality were published in 2020.3,4 These reviews include studies conducted in all parts of the world and across a wide range of exposure levels. The linear summary estimates from these global systematic reviews are used in the current HIA and CBA informing the revision of the EU AAQD. The systematic review on PM2.5 and total mortality documented a summary estimate of 1.08 per 10 μg/m3 with a confidence interval of (1.06, 1.09), based on 25 studies.3 The systematic review on NO2 and total mortality reported a summary estimate of 1.02 per 10 μg/m3 with a confidence interval of (1.01, 1.04), based on 24 studies.4 This latter review has also reported an association between longterm, warm season ozone exposure and total mortality with a summary effect estimate of 1.01 (1.00, 1.02) per 10 μg/m3, which is being used to estimate the impacts of long-term warm season ozone concentrations in the revision of the EU AAQD. These systematic reviews were published in 2020 and included studies available until September 2018. They do not include important new European studies that have been published since. We propose that additional analyses should be conducted based on these new studies to ensure that the HIA and CBA to inform the revision of the EU AAQD considers the most recent and relevant evidence. We suggest using effect estimates from recent European studies only, as these are the most relevant to estimating impacts and benefits for recent European exposure levels and populations. While studies conducted outside of Europe form an important part of the overall evidence base, when quantifying risks in Europe, it is important to use exposure-response estimates from epidemiologic studies that reflect European population demographics, air quality and exposure patterns, healthcare systems (particularly for outcomes based on administrative databases), and baseline mortality and morbidity rates. Geographical restriction for HIA and CBA purposes is common practice in many other countries, including the policy assessment for the review of National Ambient Air Quality Standards in the United States. We recommend the use of the exposure-response relationship estimates from ELAPSE for these additional analyses. ELAPSE is the largest study in Europe by far, designed specifically to address the effects of exposure to low levels of air pollution—below current EU air quality limit values—and represents the latest and most relevant data for Europe. ELAPSE has estimated associations between long-term exposure to air pollution and mortality using two approaches: a pooled cohort of over 325,000 persons from eight cohorts from six EU countries, published in Strak et al,5 and analyses of 28 million people from seven large administrative nationwide (Denmark, Netherlands, Norway, United Kingdom, Switzerland, Belgium) and citywide (Rome) cohorts, published in Stafoggia et al.6 The pooled cohort had access to detailed information, such as smoking, physical activity, body mass index, and alcohol intake. The very large administrative cohorts have less detailed information on lifestyle and social factors, and they used an “indirect” approach to account for those factors in the analyses. ELAPSE includes data on a very large number of participants in 11 European countries in total, almost all of whom were exposed to levels of PM2.5 and NO2 aInstitute for Occupational, Social and Environmental Medicine, Medical Faculty, Heinrich Heine University of Düsseldorf, Düsseldorf, Germany, and European Respiratory Society (ERS); bInstitute for Risk Assessment Sciences, Utrecht University, Utrecht, The Netherlands; cDepartment of Public Health, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark, and European Respiratory Society (ERS); dEnvironmental Research Group, School of Public Health, Imperial College, London, United Kingdom; and eHealth Effects Institute, Boston, MA, and International Society for Environmental Epidemiology (ISEE)
欧洲未来清洁空气政策的好处:PM2.5和二氧化氮对死亡率影响的拟议分析。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Environmental Epidemiology
Medicine-Public Health, Environmental and Occupational Health
CiteScore
5.70
自引率
2.80%
发文量
71
审稿时长
25 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


