Change in hospitalization rates following transcatheter left atrial appendage occlusion.
Archives of Medical Sciences. Atherosclerotic Diseases
Pub Date : 2021-12-10
eCollection Date: 2021-01-01
DOI:10.5114/amsad.2021.111405
引用次数: 0
Abstract
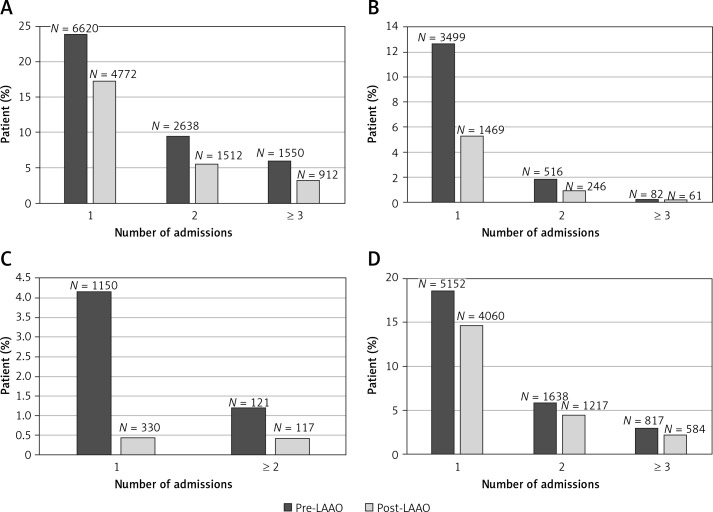
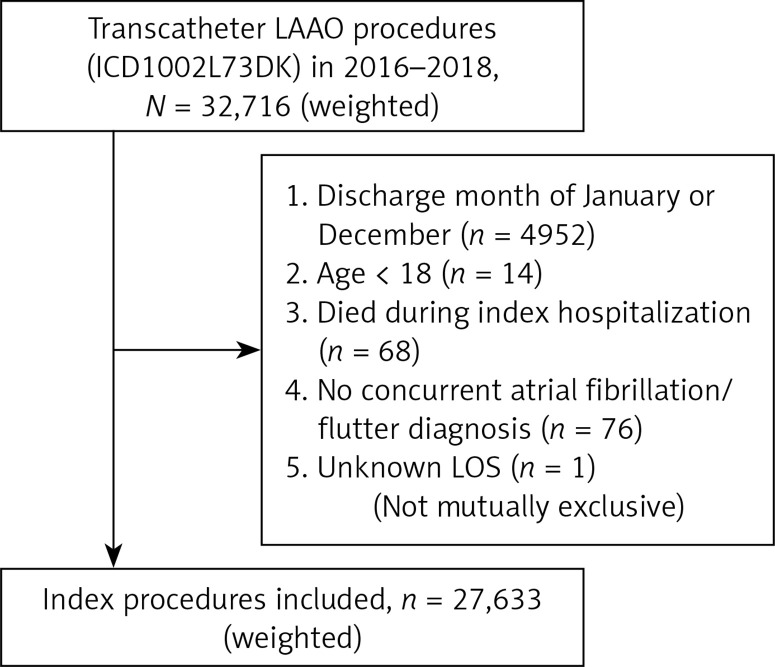
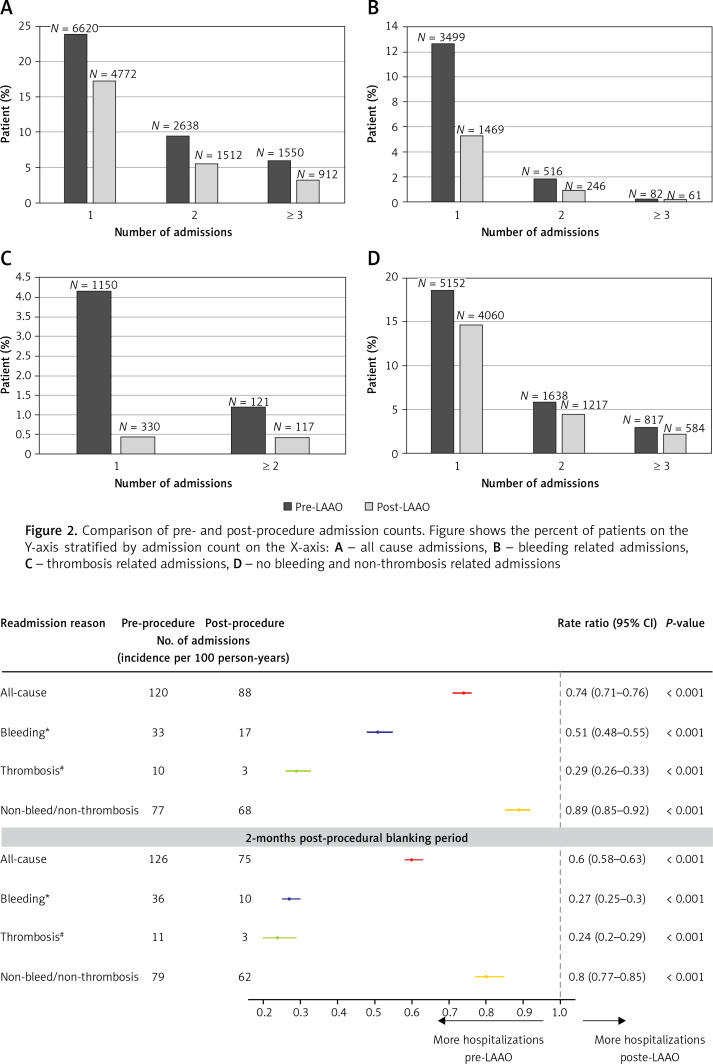
Introduction Left atrial appendage occlusion (LAAO) is recommended in patients with non-valvular atrial fibrillation (AF) who have contraindications to or are intolerant of long-term oral anticoagulants (OAC), but its impact on hospitalization rates has not been well described. The objective of our study is to describe the incidence of all-cause, bleeding-related, and thrombosis-related hospitalizations before and after LAAO. Material and methods We used the Nationwide Readmission Database to include patients aged ≥ 18 years with a diagnosis of AF who underwent transcatheter LAAO during the months of February-November in each year between 2016 and 2018. Patients who died during the index procedure or had missing length of hospital stay or mortality information were excluded. Results A total of 27,633 patients were included (median age: 77 years, 41% female) with an average pre- and post-LAAO monitoring period of 6.5 and 5.5 months respectively. Of these, 10,808 (39.1%) patients had one or more admissions prior to the procedure compared to 7,196 (26.0%) after the procedure. There was a 26% reduction in incidence of all-cause admissions (rate ratio (RR) = 0.74, 95% confidence interval (CI): 0.71–0.76; p < 0.001), 49% reduction in bleeding-related admissions (RR = 0.51, 95% CI: 0.48–0.55; p < 0.001), and 71% reduction in thrombosis-related readmissions (RR = 0.29, 95% CI: 0.26–0.33; p < 0.001) after LAAO. Conclusions In a contemporary, nationally representative dataset, we found that LAAO is associated with a significant decrease in all-cause, bleeding-related, and thrombosis-related admissions. These findings lend support to the current use of transcatheter LAAO in clinical practice for patients with contraindications to OAC and/or at high risk of bleeding.
经导管左心耳闭塞后住院率的变化。
左心耳闭塞(LAAO)被推荐用于有禁忌症或不耐受长期口服抗凝剂(OAC)的非瓣膜性心房颤动(AF)患者,但其对住院率的影响尚未得到很好的描述。我们研究的目的是描述LAAO前后全因、出血相关和血栓相关住院的发生率。材料和方法:我们使用全国再入院数据库纳入了年龄≥18岁、诊断为房颤且在2016年至2018年每年2月至11月接受经导管LAAO的患者。在索引程序中死亡或缺少住院时间或死亡率信息的患者被排除在外。结果:共纳入27,633例患者(中位年龄:77岁,女性41%),laao前后平均监测时间分别为6.5个月和5.5个月。其中,10,808例(39.1%)患者在手术前有一次或多次入院,而手术后有7,196例(26.0%)。全因入院发生率降低26% (RR = 0.74, 95%可信区间(CI): 0.71-0.76;p < 0.001),出血相关入院减少49% (RR = 0.51, 95% CI: 0.48-0.55;p < 0.001),血栓相关再入院减少71% (RR = 0.29, 95% CI: 0.26-0.33;p < 0.001)。结论:在当代具有全国代表性的数据集中,我们发现LAAO与全因、出血相关和血栓相关入院的显著减少有关。这些发现支持了目前在临床实践中对OAC禁忌症和/或出血高风险患者使用经导管LAAO的做法。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


