A Prediction Nomogram Combining Epworth Sleepiness Scale and Other Clinical Parameters to Predict Obstructive Sleep Apnea in Patients with Hypertension.
IF 1.7
4区 医学
Q3 PERIPHERAL VASCULAR DISEASE
International Journal of Hypertension
Pub Date : 2022-08-05
eCollection Date: 2022-01-01
DOI:10.1155/2022/3861905
引用次数: 0
Abstract
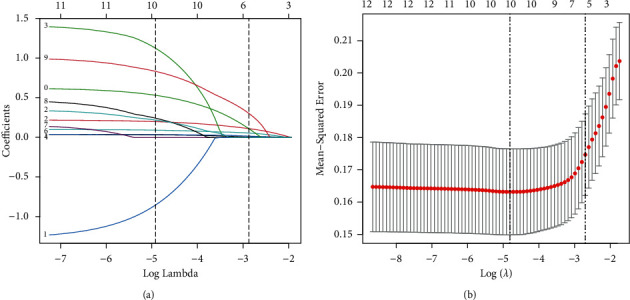
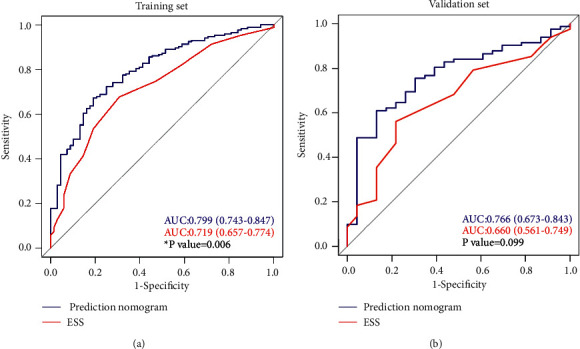
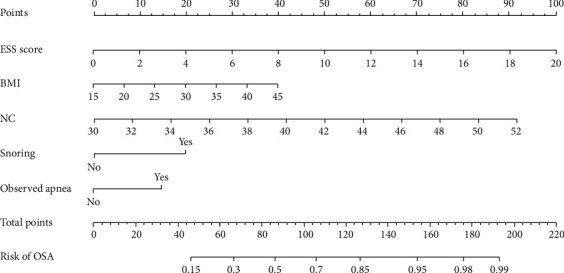
Background Obstructive sleep apnea (OSA) is common in patients with hypertension. Nonetheless, OSA is underdiagnosed despite considerable evidence of the association between OSA and adverse health outcomes. This study developed and validated a clinical nomogram to predict OSA in patients with hypertension based on the Epworth Sleepiness Scale (ESS) score and OSA-related parameters. Methods A total of 347 hypertensive patients with suspected OSA were retrospectively enrolled and randomly assigned to a training set and a validation set at 70 : 30 (N = 242/N = 105) ratio. OSA was diagnosed through sleep monitoring and was defined as an apnea-hypopnea index ≥5 events/h. Using the least absolute shrinkage and selection operator regression model, we identified potential predictors of OSA and constructed a nomogram model in the training set. The predictive performance of the nomogram was assessed and validated by discrimination and calibration. The nomogram was also compared with ESS scores according to decision curve analysis (DCA), integrated discrimination index (IDI), and net reclassification index (NRI). Results ESS scores, body mass index, neck circumference, snoring, and observed apnea predicted OSA are considered. The nomogram showed similar discrimination between the training set (AUC: 0.799, 95% CI: 0.743–0.847) and validation set (AUC: 0.766, 95% CI: 0.673–0.843) and good calibration in the training (P=0.925 > 0.05) and validation (P=0.906 > 0.05) sets. Compared with the predictive value of the ESS, the nomogram was clinically useful and significantly improved reclassification accuracy (NRI: 0.552, 95% CI: 0.282–0.822, P < 0.001; IDI: 0.088, 95% CI: 0.045–0.133, P < 0.001) at a probability threshold of >42%. Conclusions We developed a novel OSA prediction nomogram based on ESS scores and OSA-related parameters. This nomogram may help improve clinical decision-making, especially in communities and primary clinics, where polysomnography is unavailable.
结合Epworth嗜睡量表及其他临床参数预测高血压患者阻塞性睡眠呼吸暂停的Nomogram。
背景:阻塞性睡眠呼吸暂停(OSA)在高血压患者中很常见。然而,尽管有大量证据表明阻塞性睡眠呼吸暂停与不良健康结果之间存在关联,但仍未得到充分诊断。本研究基于Epworth嗜睡量表(ESS)评分和OSA相关参数,开发并验证了预测高血压患者OSA的临床nomogram。方法:回顾性纳入347例疑似OSA的高血压患者,按70:30 (N = 242/N = 105)的比例随机分为训练组和验证组。通过睡眠监测诊断OSA,并将其定义为呼吸暂停-低通气指数≥5次/小时。使用最小绝对收缩和选择算子回归模型,我们确定了OSA的潜在预测因子,并在训练集中构建了nomogram模型。通过判别和校准来评估和验证nomogram预测性能。并根据决策曲线分析(DCA)、综合判别指数(IDI)和净重分类指数(NRI)将nomogram与ESS评分进行比较。结果:考虑ESS评分、体重指数、颈围、打鼾和观察到的呼吸暂停预测OSA。训练集(AUC: 0.799, 95% CI: 0.743-0.847)和验证集(AUC: 0.766, 95% CI: 0.673-0.843)之间的判别相似,训练集(P=0.925 > 0.05)和验证集(P=0.906 > 0.05)校准良好。与ESS的预测值相比,nomogram临床应用价值显著提高(NRI: 0.552, 95% CI: 0.282 ~ 0.822, P < 0.001;IDI: 0.088, 95% CI: 0.045-0.133, P < 0.001),概率阈值>42%。结论:我们开发了一种基于ESS评分和OSA相关参数的新的OSA预测图。这种图可能有助于改善临床决策,特别是在社区和初级诊所,在那里多导睡眠图是不可用的。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
International Journal of Hypertension
Medicine-Internal Medicine
CiteScore
4.00
自引率
5.30%
发文量
45
期刊介绍:
International Journal of Hypertension is a peer-reviewed, Open Access journal that provides a forum for clinicians and basic scientists interested in blood pressure regulation and pathophysiology, as well as treatment and prevention of hypertension. The journal publishes original research articles, review articles, and clinical studies on the etiology and risk factors of hypertension, with a special focus on vascular biology, epidemiology, pediatric hypertension, and hypertensive nephropathy.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


