Chordoid meningioma in a pediatric patient with tuberous sclerosis complex.
Korean Journal of Pathology
Pub Date : 2014-08-01
Epub Date: 2014-08-26
DOI:10.4132/KoreanJPathol.2014.48.4.302
引用次数: 4
Abstract
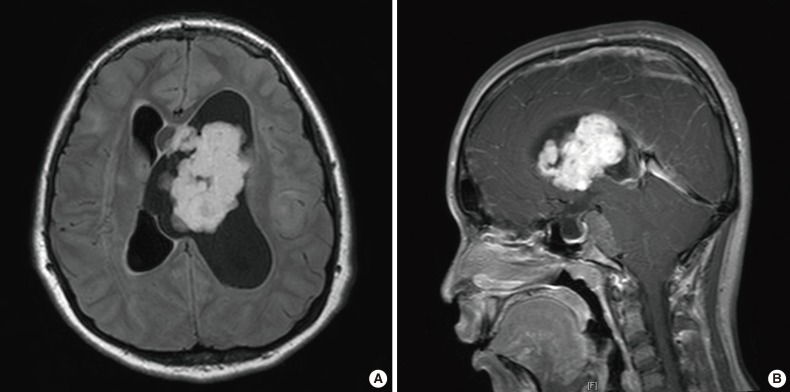
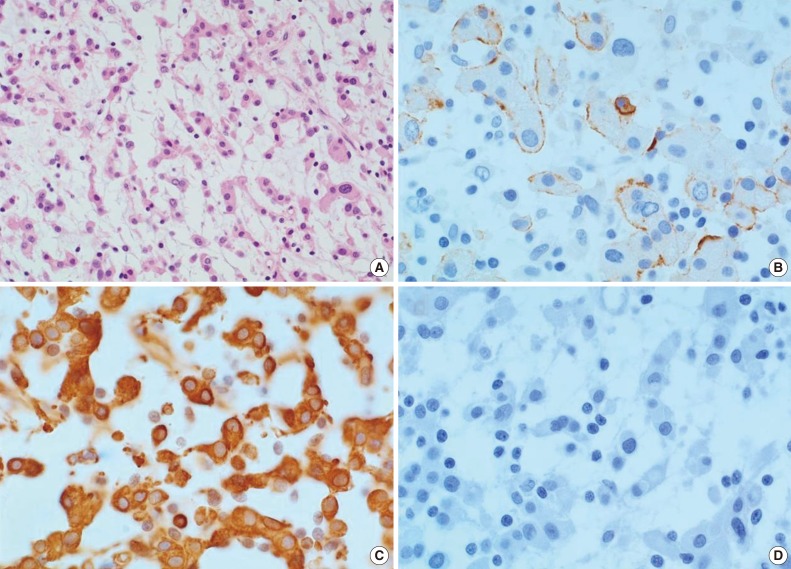
Meningeal tumors are rare in childhood, comprising less than 4.2% of all pediatric primary intracranial tumors.1 Fourteen histological subtypes of meningiomas exist in the World Health Organization (WHO) classification system.2 Chordoid meningioma (CM) is a rare meningiomal variant characterized histologically by features that mimic chordoma and other chordoid neoplasms.2 Chordoid meningiomal tumors tend to exhibit local recurrence and aggressive behavior, although they typically show morphologically benign features. In a tuberous sclerosis complex (TSC) patient, hamartomas can occur in multiple organs and cause diverse clinical symptoms. Cortical tubers, subependymal nodules (SENs) and subependymal giant cell astrocytomas (SEGAs) are representative lesions of TSC and can be detected by magnetic resonance imaging (MRI) of the brain.3 SEGA lesions have been found to occur in approximately 6.1% to 18.5% of TSC patients, and account for 90% of all intracranial tumors associated with TSC.4 SEGA lesions are commonly located in the foramen of Monro or the periventricular region,5 and can cause loss of vision, papillary edemas, intracranial calcification, and hydrocephalus.6 The primary method for treating SEGA lesions consists of surgical resection of the tumors; complete and early surgical removal of tumors has been shown to be the most important prognostic factor.6 Childhood CM has been shown to account for only ~0.5-1% of all meningiomas, with intraventricular occurrence of CM reported in only 27 children to date.2,7 Also, CM has not been reported in any TSC patients to date. Here we report a case of intraventricular CM, which appeared highly similar to SEGA in brain MRI scans, in a child with TSC.
小儿结节性硬化症合并脊索样脑膜瘤1例。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


