Laparoscopic versus Open Complete Mesocolic Excision for Right Colon Cancer.
IF 1.6
Q4 ONCOLOGY
International Journal of Surgical Oncology
Pub Date : 2021-02-02
eCollection Date: 2021-01-01
DOI:10.1155/2021/8859879
引用次数: 8
Abstract
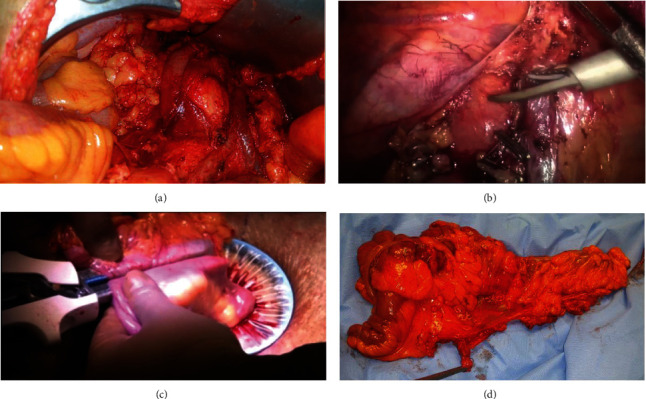
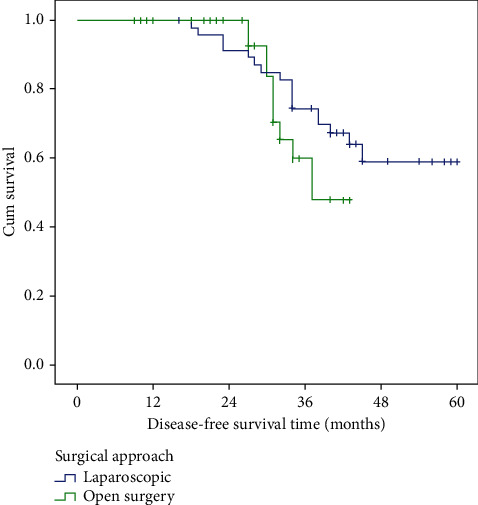
Results The mean operative time was significantly longer in the LCME group than that in the OCME group with less mean intraoperative blood loss. Conversion was required in 4 patients (8.3%) in the LCME group. The use of laparoscopy increased the number of harvested lymph nodes compared to the open approach (39.81 ± 16.74 vs. 32.65 ± 12.28, respectively, P=0.010). The laparoscopic approach was associated with a shorter time interval to first flatus as well as shorter time interval to liquid and normal diet after surgery. The postoperative hospital stay was significantly shorter in the LCME group. The complication rate was slightly lower in the LCME (14.7%) than in the OCME group (27.2%) (P=0.252). The 3-year OS in the LCME group was similar to that in OCME (78.2% vs. 63.2%, respectively, P value = 0.423). The three-year DFS in the laparoscopic group was higher (74.5%) than the open group (60.0%), but did not reach statistical significance (P value = 0.266). Conclusions In conclusion, laparoscopic CME right hemicolectomy is a technically feasible and safe procedure if surgeon expertise is present. LCME has long-term oncologic outcomes (recurrence and survival) comparable to open surgery for management of patients with stage II or III colon cancer.
腹腔镜与开放式结肠系膜全切除术治疗右结肠癌。
结果:LCME组平均手术时间明显长于OCME组,平均术中出血量较少。在LCME组中,有4例患者(8.3%)需要转换。腹腔镜较开放入路淋巴结清扫数增加(分别为39.81±16.74比32.65±12.28,P=0.010)。腹腔镜入路与术后首次放屁的时间间隔较短,与术后液体和正常饮食的时间间隔较短有关。LCME组术后住院时间明显缩短。LCME组的并发症发生率(14.7%)略低于OCME组(27.2%)(P=0.252)。LCME组3年OS与OCME组相似(分别为78.2% vs. 63.2%, P值= 0.423)。腹腔镜组3年DFS(74.5%)高于开放组(60.0%),但差异无统计学意义(P值= 0.266)。结论:总之,如果有外科医生的专业知识,腹腔镜CME右半结肠切除术在技术上是可行和安全的。LCME具有与开放手术治疗II期或III期结肠癌患者相当的长期肿瘤预后(复发和生存)。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
3.70
自引率
0.00%
发文量
5
审稿时长
20 weeks
期刊介绍:
International Journal of Surgical Oncology is a peer-reviewed, Open Access journal that publishes original research articles, review articles, and clinical studies in all areas of surgical oncology.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


