Effects of vitamin K2 and D3 supplementation on epicardial adipose tissue and systemic inflammation: A substudy of the AVADEC trial
IF 5.7
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background and aims
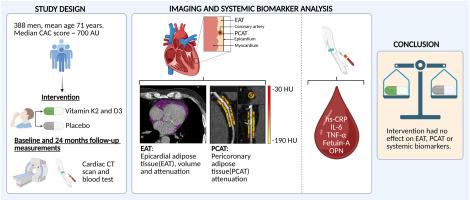
Vitamins K2 and D3 may improve cardiovascular health by modulating inflammation and vascular calcification. Inflammation contributes to atherosclerosis and can be assessed through imaging and systemic biomarkers. This study investigated whether vitamin K2 and D3 supplementation reduces inflammation in epicardial adipose tissue (EAT), including pericoronary adipose tissue (PCAT), and systemic inflammation in elderly men at cardiovascular risk.
Methods
In the Aortic Valve DECalcification (AVADEC) trial, 388 men aged 65–74 received daily vitamin K2 (720 μg) and D3 (25 μg) or placebo for 24 months. EAT inflammation was assessed using non-contrast CT [EAT volume and attenuation] and contrast-enhanced CT [PCAT attenuation]. Systemic inflammation was evaluated via hs-CRP, IL-6, TNF-α, Fetuin-A, and osteopontin (OPN). Dephosphorylated uncarboxylated matrix Gla protein (dp-ucMGP), the inactive form of MGP, served as a proxy for vitamin K2 status.
Results
After 24 months, EAT volume increased in the placebo group (Δ5.66 cm3,95% CI 1.35; 9.98) and non-significantly in the vitamin group (Δ3.44 cm3, 95% CI -0.44; 7.33), with an intergroup difference of −2.22 cm3 (95% CI -8.01; 3.57). EAT attenuation declined similarly (intergroup difference: 0.32 HU, 95% CI -0.23; 0.87). PCAT attenuation remained unchanged. No significant changes were seen in systemic markers, though OPN increased modestly in the vitamin group (Δ25.72 pg/mL, 95% CI 2.40; 49.05). dp-ucMGP decreased significantly with supplementation (intergroup difference: 255.31 pmol/L, 95% CI -289.56; −221.05).
Conclusions
Despite reduction in dp-ucMGP, high-dose vitamin K2 and D3 supplementation did not affect EAT, PCAT or systemic inflammation over 24 months. Alternative strategies may be needed to target inflammatory pathways in cardiovascular disease prevention.
维生素K2和D3补充对心外膜脂肪组织和全身性炎症的影响:AVADEC试验的一项亚研究
背景和目的:维生素K2和D3可能通过调节炎症和血管钙化来改善心血管健康。炎症有助于动脉粥样硬化,可以通过成像和系统生物标志物进行评估。本研究调查了维生素K2和D3补充剂是否能减少心血管风险老年男性心外膜脂肪组织(EAT),包括冠状动脉周围脂肪组织(PCAT)的炎症和全身炎症。方法:在主动脉瓣脱钙(AVADEC)试验中,388名65-74岁的男性每天服用维生素K2 (720 μg)和D3 (25 μg)或安慰剂,持续24个月。通过非对比CT [EAT体积和衰减]和对比增强CT [PCAT衰减]评估EAT炎症。通过hs-CRP、IL-6、TNF-α、Fetuin-A和骨桥蛋白(OPN)评估全身性炎症。去磷酸化非羧化基质Gla蛋白(dp-ucMGP)是MGP的非活性形式,可作为维生素K2状态的代理。结果:24个月后,安慰剂组的EAT体积增加(Δ5.66 cm3,95% CI 1.35; 9.98),维生素组的EAT体积增加(Δ3.44 cm3,95% CI -0.44; 7.33),组间差异为-2.22 cm3 (95% CI -8.01; 3.57)。EAT衰减同样下降(组间差异:0.32 HU, 95% CI -0.23; 0.87)。PCAT衰减保持不变。虽然维生素组的OPN略有增加(Δ25.72 pg/mL, 95% CI 2.40; 49.05),但系统标志物未见显著变化。添加后dp-ucMGP显著降低(组间差异:255.31 pmol/L, 95% CI: -289.56; -221.05)。结论:尽管dp-ucMGP降低,高剂量维生素K2和D3补充在24个月内对EAT、PCAT或全身性炎症没有影响。可能需要其他策略来针对心血管疾病预防中的炎症途径。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Atherosclerosis
医学-外周血管病
CiteScore
9.80
自引率
3.80%
发文量
1269
审稿时长
36 days
期刊介绍:
Atherosclerosis has an open access mirror journal Atherosclerosis: X, sharing the same aims and scope, editorial team, submission system and rigorous peer review.
Atherosclerosis brings together, from all sources, papers concerned with investigation on atherosclerosis, its risk factors and clinical manifestations. Atherosclerosis covers basic and translational, clinical and population research approaches to arterial and vascular biology and disease, as well as their risk factors including: disturbances of lipid and lipoprotein metabolism, diabetes and hypertension, thrombosis, and inflammation. The Editors are interested in original or review papers dealing with the pathogenesis, environmental, genetic and epigenetic basis, diagnosis or treatment of atherosclerosis and related diseases as well as their risk factors.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


