Chinese herbal medicine alleviates renal impairment induced by immunosuppressants in patients post living donor liver transplantation
IF 3
3区 医学
Q1 INTEGRATIVE & COMPLEMENTARY MEDICINE
Journal of Traditional and Complementary Medicine
Pub Date : 2025-10-01
DOI:10.1016/j.jtcme.2024.09.004
引用次数: 0
Abstract
Background and aim
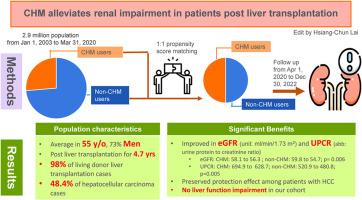
Patients post liver transplantation (LT) with long-term immunosuppression agents will suffer from renal function impairment. Chinese herbal medicine (CHM) has been reported to relieve chronic kidney disease progression. Nevertheless, there are a lack of high-quality reports related to CHM reducing renal dysfunction in post-LT patients. We aim to investigate whether CHM alleviates renal impairment induced by immunosuppressants in patients having undergone LT.
Materials and methods
We conducted a hospital-based retrospective cohort study including patients with LT from January 1, 2003 to March 31, 2020. We matched the CHM users to non-users at a 1:1 ratio according to baseline variables, comorbidities and drug use status by propensity score (PS) matching.
Results
The study enrolled a total of 1052 LT patients. After PS matching, 554 patients were included with a 1:1 ratio. CHM and non-CHM users exhibited a significant difference of improved urine protein to creatinine ratio (UPCR) over several 3-month follow-up periods. CHM users exhibited an alleviated decrease in GFR compared to non-CHM users after 12 months of follow-up (CHM: 58.1 to 56.3 ml/min/1.73 m2; non-CHM: 59.8 to 54.7 ml/min/1.73 m2). Among HCC patients, CHM users had alleviated GFR, UPCR and blood urea nitrogen impairments compared to non-CHM users. The most commonly prescribed herbs and formulas are noted.
Conclusion
We herein report that CHM could protect renal function after 12 months of follow-up compared to non-CHM users, without liver function impairment. However, the long-term effects and exact renal protection mechanisms require further investigations to confirm.
中药对活体肝移植后免疫抑制剂所致肾损害的缓解作用
背景与目的肝移植术后长期使用免疫抑制剂的患者会出现肾功能损害。据报道,中草药(CHM)可以缓解慢性肾脏疾病的进展。然而,目前还缺乏高质量的关于CHM降低肾移植后患者肾功能的报道。我们的目的是研究中草药是否能减轻肝移植患者免疫抑制剂引起的肾损害。材料和方法我们进行了一项基于医院的回顾性队列研究,纳入了2003年1月1日至2020年3月31日的肝移植患者。根据基线变量、合并症和药物使用状况,通过倾向评分(PS)匹配,我们将CHM使用者与非使用者按1:1的比例进行匹配。结果本研究共纳入1052例LT患者。PS匹配后,按1:1比例纳入554例患者。在几个3个月的随访期间,CHM和非CHM使用者表现出尿蛋白与肌酐比率(UPCR)改善的显著差异。随访12个月后,与非CHM使用者相比,CHM使用者的GFR下降有所缓解(CHM: 58.1至56.3 ml/min/1.73 m2;非CHM: 59.8至54.7 ml/min/1.73 m2)。在HCC患者中,与未使用中草药的患者相比,中草药使用者的GFR、UPCR和血尿素氮损伤有所减轻。最常用的草药和配方被注意到。结论与未使用中草药的患者相比,经过12个月的随访,中草药可以保护肾功能,无肝功能损害。然而,长期的影响和确切的肾脏保护机制需要进一步的研究来证实。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Traditional and Complementary Medicine
Medicine-Complementary and Alternative Medicine
CiteScore
9.30
自引率
6.70%
发文量
78
审稿时长
66 days
期刊介绍:
eJTCM is committed to publish research providing the biological and clinical grounds for using Traditional and Complementary Medical treatments as well as studies that demonstrate the pathophysiological and molecular/biochemical bases supporting the effectiveness of such treatments. Review articles are by invitation only.
eJTCM is receiving an increasing amount of submission, and we need to adopt more stringent criteria to select the articles that can be considered for peer review. Note that eJTCM is striving to increase the quality and medical relevance of the publications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


