The role of neuromodulation in heart failure with preserved ejection fraction
IF 3.3
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
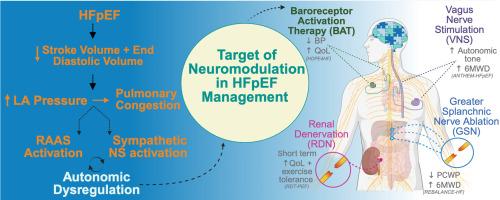
Heart failure with preserved ejection fraction (HFpEF) is a clinical syndrome with limited treatment options to improve long-term outcomes such as quality of life, exercise capacity, and mortality. Neuromodulation-based therapies have emerged as potential interventions to address autonomic dysregulation in HFpEF. This review discusses the long-term efficacy and safety of four key neuromodulation therapies: Renal Denervation (RDN), Baroreceptor Activation Therapy (BAT), Vagus Nerve Stimulation (VNS), and Greater Splanchnic Nerve (GSN) Ablation. Each therapy shows promise, but variability exists in terms of patient outcomes, procedural risks, and long-term durability. This paper evaluates the pros and cons of each approach, focusing on their potential to improve clinical outcomes in diverse HFpEF phenotypes.
Objective
To summarise and critically assess the role of neuromodulation-based devices in managing HFpEF, including their mechanisms, efficacy, and impact on patient outcomes.
Methods
We reviewed clinical trials and studies involving neuromodulation therapies for HFpEF, focusing on VNS, RDN, BAT, and GSN. The review includes randomised controlled trials and feasibility studies assessing various endpoints such as functional status, QoL, exercise capacity, and adverse events.
Results
Neuromodulation therapies show potential in improving symptoms and QoL for HFpEF patients. The ANTHEM-HFpEF trial demonstrated VNS's efficacy in enhancing functional status and autonomic tone, although cardiac mechanical function showed minimal change. RSD trials, including RDT-PEF and UNLOAD-HFpEF, indicated mixed results with some improvements in symptoms and cardiac function, though limitations like sample size and device effectiveness persist. BAT, through the BAROSTIM NEO System, has shown promise in reducing sympathetic activity and improving heart failure symptoms. The GSN ablation trials indicated significant reductions in pulmonary capillary wedge pressure (PCWP) and improved exercise capacity, though further large-scale studies are needed to confirm these findings.
Conclusions
Neuromodulation-based device interventions represent a promising frontier in HFpEF management, offering potential improvements in symptoms, QoL, and functional status. However, the variability in trial outcomes and the need for further research underscore the necessity for continued investigation to fully establish the efficacy and safety of these therapies.
神经调节在保留射血分数的心力衰竭中的作用。
背景:心力衰竭伴保留射血分数(HFpEF)是一种临床综合征,治疗选择有限,无法改善长期预后,如生活质量、运动能力和死亡率。基于神经调节的疗法已成为解决HFpEF自主神经失调的潜在干预措施。本文综述了四种主要神经调节疗法的长期疗效和安全性:肾去神经(RDN)、压力受体激活疗法(BAT)、迷走神经刺激(VNS)和大膈神经(GSN)消融。每种疗法都显示出希望,但在患者预后、手术风险和长期持久性方面存在差异。本文评估了每种方法的优缺点,重点关注它们在改善不同HFpEF表型的临床结果方面的潜力。目的:总结和批判性评估基于神经调节的装置在HFpEF治疗中的作用,包括其机制、疗效和对患者预后的影响。方法:我们回顾了有关HFpEF神经调节疗法的临床试验和研究,重点是VNS、RDN、BAT和GSN。该综述包括随机对照试验和可行性研究,评估各种终点,如功能状态、生活质量、运动能力和不良事件。结果:神经调节疗法可改善HFpEF患者的症状和生活质量。ANTHEM-HFpEF试验证实了VNS在增强功能状态和自主神经张力方面的有效性,尽管心脏机械功能的变化很小。RSD试验,包括RDT-PEF和UNLOAD-HFpEF,显示出混合的结果,症状和心功能有所改善,尽管样本量和装置有效性等限制仍然存在。BAT通过BAROSTIM NEO系统,在减少交感神经活动和改善心力衰竭症状方面显示出希望。GSN消融试验显示肺毛细血管楔压(PCWP)显著降低,运动能力提高,但需要进一步的大规模研究来证实这些发现。结论:基于神经调节的装置干预是HFpEF管理的一个有前景的前沿,可以改善症状、生活质量和功能状态。然而,试验结果的可变性和进一步研究的必要性强调了继续调查以充分确定这些疗法的有效性和安全性的必要性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Current Problems in Cardiology
医学-心血管系统
CiteScore
4.80
自引率
2.40%
发文量
392
审稿时长
6 days
期刊介绍:
Under the editorial leadership of noted cardiologist Dr. Hector O. Ventura, Current Problems in Cardiology provides focused, comprehensive coverage of important clinical topics in cardiology. Each monthly issues, addresses a selected clinical problem or condition, including pathophysiology, invasive and noninvasive diagnosis, drug therapy, surgical management, and rehabilitation; or explores the clinical applications of a diagnostic modality or a particular category of drugs. Critical commentary from the distinguished editorial board accompanies each monograph, providing readers with additional insights. An extensive bibliography in each issue saves hours of library research.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


