Clinical, economic, and health care resource utilization burden of acute myocardial infarction and the role of systemic inflammation in US hospitals: A real-world study
IF 5.9
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
Acute myocardial infarction (AMI), a leading cause of death in the US, is associated with significant clinical and economic burden. Systemic inflammation is a risk factor for worse cardiovascular outcomes, but the role of systemic inflammation in patients with AMI is not well established.
Objective
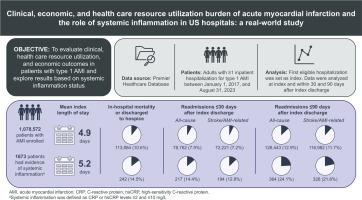
To evaluate clinical, health care resource utilization (HCRU), and economic outcomes in patients with type 1 AMI, and explore results based on systemic inflammation status.
Methods
Data from the Premier Healthcare Database were retrospectively analyzed, including adults with ≥1 inpatient hospitalization for type 1 AMI (using ICD-10-CM codes) from January 1, 2017, to August 31, 2023. Data were analyzed at index and within 30 and 90 days after index discharge. Demographics, clinical and HCRU outcomes, and costs were described for all patients with AMI and compared between those with and without evidence of systemic inflammation. Inflammation status was based on C-reactive protein (CRP) or high-sensitivity C-reactive protein (hsCRP) levels, such that patients with CRP/hsCRP between 2 and 10 mg/L were considered to have evidence of systemic inflammation. Patients with levels <2 mg/L or without CRP/hsCRP test results were considered to have no evidence of systemic inflammation. CRP/hsCRP test results were available in a limited number of patients.
Results
Among patients with AMI (N = 1,078,572), in-hospital mortality was 7.6 % during index hospitalization. The mean index length of stay was 5 days, and average cost of care was $23,648. Readmission rates were 7.9 % and 12.9 % within 30 and 90 days after discharge, respectively. Patients with evidence of systemic inflammation (n = 1673) had higher mortality and longer index stays as well as increased readmission rates compared with patients without evidence of systemic inflammation (n = 1,076,899) (all, P < 0.01).
Conclusion
Patients experiencing AMI, and especially those with evidence of systemic inflammation, experience persistently high risk of mortality, morbidity, recurrence, and large economic burdens. Greater attention is needed to optimize the care of this at-risk population.
美国医院急性心肌梗死的临床、经济和卫生保健资源利用负担和全身性炎症的作用:一项真实世界的研究
背景:急性心肌梗死(AMI)是美国的主要死亡原因之一,与重大的临床和经济负担相关。全身性炎症是心血管预后恶化的危险因素,但全身性炎症在AMI患者中的作用尚不明确。目的评价1型AMI患者的临床、医疗资源利用(HCRU)和经济预后,并探讨基于全身性炎症状态的结果。方法回顾性分析来自Premier Healthcare数据库的数据,包括2017年1月1日至2023年8月31日期间因1型AMI(使用ICD-10-CM代码)住院≥1例的成年人。数据分析在指数和指数排出后30天和90天内的数据。描述了所有AMI患者的人口统计学、临床和HCRU结果和费用,并比较了有和没有全身性炎症证据的患者。炎症状态基于c反应蛋白(CRP)或高敏c反应蛋白(hsCRP)水平,因此CRP/hsCRP在2 - 10mg /L之间的患者被认为有全身性炎症的证据。2 mg/L水平或没有CRP/hsCRP测试结果的患者被认为没有全身性炎症的证据。CRP/hsCRP检测结果在有限数量的患者中可用。结果AMI患者(N = 1,078,572)在指数住院期间的住院死亡率为7.6%。平均指数住院时间为5天,平均护理费用为23,648美元。出院后30天和90天再入院率分别为7.9%和12.9%。有全身性炎症证据的患者(n = 1673)与无全身性炎症证据的患者(n = 1,076,899)相比,死亡率更高,住院时间更长,再入院率也更高(均P <; 0.01)。结论AMI患者,特别是有全身性炎症的患者,死亡率、发病率、复发率持续高,经济负担大。需要更加重视优化对这一高危人群的护理。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

American journal of preventive cardiology
Cardiology and Cardiovascular Medicine
CiteScore
6.60
自引率
0.00%
发文量
0
审稿时长
76 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


