Prognostic impact of cardiac dysfunctions in patients with ST-segment elevation myocardial infarction
IF 1.8
Q3 CARDIAC & CARDIOVASCULAR SYSTEMS
American heart journal plus : cardiology research and practice
Pub Date : 2025-10-02
DOI:10.1016/j.ahjo.2025.100628
引用次数: 0
Abstract
Background
The incidence and impact of cardiac dysfunctions after ST-segment elevation myocardial infarction (STEMI) are not understood. We aimed to characterize the prevalence of follow-up systolic and diastolic dysfunction and their associations with long-term outcomes after STEMI.
Methods and results
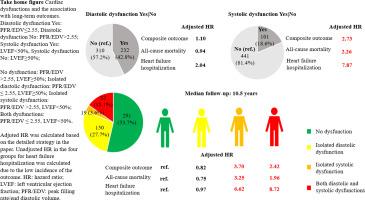
This sub-study of the DANAMI-3 trial included 542 patients with STEMI. Cardiac magnetic resonance (CMR)-defined systolic/diastolic impairment was applied to define systolic/diastolic dysfunction. Systolic dysfunction was defined as left ventricular ejection fraction (LVEF) < 50 %, and diastolic dysfunction as peak filling rate/end-diastolic volume (PFR/EDV) ≤ 2.55 by CMR three months after STEMI. The primary outcome was a composite of all-cause mortality and hospitalization for heart failure. Secondary outcomes were individual components of the primary outcome. During a median follow-up of 10.5 years, 103 patients died or were hospitalized for heart failure. A total of 101 and 232 patients had systolic and diastolic dysfunction at three months. Cox regression showed that LVEF was significantly associated with the outcomes, while PFR/EDV was not associated with any outcome. Systolic dysfunction (LVEF<50 %) was associated with the primary endpoint (adjusted hazards ratio [HR] 2.73), all-cause mortality (aHR 2.26), and hospitalization for heart failure (aHR 7.87). The incidences of isolated diastolic dysfunction, isolated systolic dysfunction and both cardiac dysfunctions were 150, 19 and 82. Patients with isolated systolic dysfunction and both dysfunctions were associated with the outcomes.
Conclusions
Cardiac dysfunctions derived from CMR-defined systolic/diastolic impairment showed in about half of the three-month STEMI-survivors. Systolic dysfunction regardless of diastolic dysfunction is a significant predictor of long-term outcomes after STEMI.
st段抬高型心肌梗死患者心功能障碍对预后的影响
st段抬高型心肌梗死(STEMI)后心功能障碍的发生率和影响尚不清楚。我们的目的是描述STEMI后随访收缩期和舒张期功能障碍的患病率及其与长期预后的关系。方法和结果DANAMI-3试验的亚研究纳入了542例STEMI患者。心脏磁共振(CMR)定义的收缩/舒张功能障碍用于定义收缩/舒张功能障碍。收缩期功能障碍定义为左室射血分数(LVEF)≥50%,舒张期功能障碍定义为STEMI后3个月CMR峰值充盈率/舒张末期容积(PFR/EDV)≤2.55。主要结局是全因死亡率和心力衰竭住院的综合结果。次要结局是主要结局的个别组成部分。在中位10.5年的随访期间,103名患者因心力衰竭死亡或住院。三个月时,分别有101例和232例患者出现收缩和舒张功能障碍。Cox回归分析显示,LVEF与预后显著相关,而PFR/EDV与预后无相关性。收缩功能障碍(LVEF< 50%)与主要终点(校正危险比[HR] 2.73)、全因死亡率(aHR 2.26)和心力衰竭住院(aHR 7.87)相关。孤立性舒张功能障碍、孤立性收缩功能障碍和两种心功能障碍的发生率分别为150例、19例和82例。孤立性收缩功能障碍和两种功能障碍的患者与结果相关。结论:在3个月的stemi幸存者中,约有一半出现了由cmr定义的收缩期/舒张期损伤引起的心脏功能障碍。收缩期功能障碍与舒张期功能障碍无关,是STEMI术后长期预后的重要预测指标。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

American heart journal plus : cardiology research and practice
Cardiology and Cardiovascular Medicine
CiteScore
1.60
自引率
0.00%
发文量
0
审稿时长
59 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


