Pre-stroke subjective sleep quality predicts 1-year clinical outcomes in patients with ischemic stroke or transient ischemic attack: A national cohort study
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Background
Sleep quality may be a predictor of outcomes following ischemic stroke. This study aims to investigate the impact of pre-stroke subjective sleep quality on clinical outcomes in stroke patients.
Methods
Patients diagnosed with acute ischemic stroke (AIS) or transient ischemic attack (TIA) were recruited from China National Stroke Registry-III. The Pittsburgh Sleep Quality Index (PSQI) was used to evaluate pre-stroke subjective sleep quality. Cox regression was to explore the relationship between PSQI and recurrent stroke, mortality, and composite vascular events; logistic regression was used for poor functional outcome.
Results
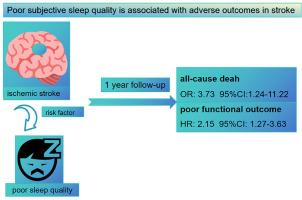
A total of 2,266 patients were enrolled. After 1 year of follow-up, 44 (1.9 %) individuals died, 180 (7.9 %) individuals experienced stroke recurrence, 195 (8.6 %) individuals experienced composite vascular events, and 172 (7.6 %) individuals had poor functional outcome. Patients in the highest quartile of PSQI score (score range: 10–20) exhibited a significantly increased risk of mortality (HR = 3.73, 95 % CI = 1.24–11.22) and poor functional outcome (OR = 2.15 95 % CI = 1.27–3.63) when compared with patients in the lowest quartile (score range: 3–5).
Conclusions
Pre-stroke poor subjective sleep quality independently predicts 1-year mortality and poor functional outcome in patients with AIS or TIA.
卒中前主观睡眠质量预测缺血性卒中或短暂性缺血性发作患者1年临床结果:一项国家队列研究
背景:睡眠质量可能是缺血性卒中预后的一个预测因子。本研究旨在探讨卒中前主观睡眠质量对卒中患者临床预后的影响。方法:从中国脑卒中国家登记iii中招募诊断为急性缺血性卒中(AIS)或短暂性脑缺血发作(TIA)的患者。采用匹兹堡睡眠质量指数(PSQI)评价脑卒中前主观睡眠质量。Cox回归探讨PSQI与卒中复发、死亡率和复合血管事件的关系;功能差的结果采用Logistic回归。结果:共纳入2266例患者。随访1年后,44人(1.9%)死亡,180人(7.9%)中风复发,195人(8.6%)出现复合血管事件,172人(7.6%)功能不良。PSQI评分最高四分位数(评分范围:10-20)的患者与评分最低四分位数(评分范围:3-5)的患者相比,死亡风险显著增加(HR = 3.73, 95% CI = 1.24-11.22),功能结局较差(OR = 2.15 95% CI = 1.27-3.63)。结论:脑卒中前主观睡眠质量差独立预测AIS或TIA患者1年死亡率和功能预后差。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


