Postoperative respiratory morbidity in chronic obstructive pulmonary disease patients receiving botulinum toxin injection before abdominal wall surgery: A multicentric study
IF 2.7
2区 医学
Q1 SURGERY
引用次数: 0
Abstract
Background
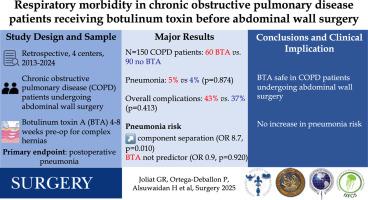
Botulinum toxin A injection is often used before abdominal wall surgery. Because botulinum toxin A inhibits the lateral abdominal muscles that have a secondary role in the breathing biomechanics, potential concerns regarding postoperative respiratory morbidity in patients with chronic obstructive pulmonary disease have been raised. This study assessed the incidence of postoperative pneumonias after abdominal wall surgery in patients with chronic obstructive pulmonary disease with and without botulinum toxin A injection.
Methods
A multicentric (4 centers) cross-sectional study was performed. Consecutive patients with chronic obstructive pulmonary disease who underwent abdominal wall surgery (2013–2024) were included. In case of large or complex hernia, botulinum toxin A was performed 4–8 weeks before surgery if judged necessary. Chronic obstructive pulmonary disease was defined based on the anesthesia preoperative consultation. The primary end point was the rate of postoperative hospital-acquired pneumonias.
Results
A total of 150 patients with chronic obstructive pulmonary disease were included: median age 68 years (interquartile range: 63–73), 61 women (41%), and median body mass index 29 kg/m2 (interquartile range: 25–33 kg/m2). Sixty patients received botulinum toxin A (40%), and 90 did not receive botulinum toxin A (60%). In the botulinum toxin A group, more patients had loss of domain (28% vs 7%, P < .001), and the median defect size was larger (12 vs 6 cm, P < .001). Fifty-four (90%) and 61 (68%) patients had midline incisional hernias in the botulinum toxin A and non–botulinum toxin A groups (P = .006). Postoperative complications occurred in 26 patients in the botulinum toxin A group (43%) and 33 patients in the non–botulinum toxin A group (37%, P = .413). Postoperative pneumonia incidences were similar in both groups (3/60 vs 4/90, P = .874). On multivariable analysis, component separation was the only predictor of pneumonia (odds ratio: 8.7, 95% confidence interval: 1.7–44.9, P = .010) and not botulinum toxin A (odds ratio: 0.9, 95% confidence interval: 0.2–4.0, P = .920).
Conclusion
Regarding postoperative respiratory morbidity, botulinum toxin A seems safe in patients with chronic obstructive pulmonary disease undergoing abdominal wall surgery.
腹壁手术前接受肉毒杆菌毒素注射的慢性阻塞性肺疾病患者术后呼吸系统发病率:一项多中心研究
背景:A型肉毒毒素注射常用于腹壁手术前。由于肉毒杆菌毒素A抑制在呼吸生物力学中起次要作用的侧腹肌,慢性阻塞性肺疾病患者术后呼吸系统发病率的潜在担忧已经提出。本研究评估了注射A型肉毒毒素和不注射A型肉毒毒素的慢性阻塞性肺疾病患者腹壁手术后肺炎的发生率。方法:采用多中心(4个中心)横断面研究。连续接受腹壁手术的慢性阻塞性肺疾病患者(2013-2024)被纳入研究。对于大疝或复杂疝,如有必要,术前4-8周进行A型肉毒杆菌毒素治疗。慢性阻塞性肺疾病的定义是基于麻醉术前咨询。主要终点是术后医院获得性肺炎的发生率。结果:共纳入150例慢性阻塞性肺疾病患者:中位年龄68岁(四分位数范围:63-73),女性61例(41%),中位体重指数29 kg/m2(四分位数范围:25-33 kg/m2)。60例患者接受了A型肉毒毒素治疗(40%),90例患者未接受A型肉毒毒素治疗(60%)。A型肉毒杆菌毒素组中,区域丧失患者较多(28% vs 7%, P < 0.001),中位缺损尺寸较大(12 vs 6 cm, P < 0.001)。肉毒毒素A组和非肉毒毒素A组分别有54例(90%)和61例(68%)发生中线切口疝(P = 0.006)。A肉毒毒素组26例(43%),非A肉毒毒素组33例(37%,P = 0.413)。两组术后肺炎发生率相似(3/60 vs 4/90, P = 0.874)。在多变量分析中,成分分离是肺炎的唯一预测因子(优势比:8.7,95%可信区间:1.7-44.9,P = 0.010),而不是肉毒杆菌毒素A(优势比:0.9,95%可信区间:0.2-4.0,P = 0.920)。结论:对于慢性阻塞性肺疾病腹壁手术患者,A型肉毒杆菌毒素似乎是安全的。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Surgery
医学-外科
CiteScore
5.40
自引率
5.30%
发文量
687
审稿时长
64 days
期刊介绍:
For 66 years, Surgery has published practical, authoritative information about procedures, clinical advances, and major trends shaping general surgery. Each issue features original scientific contributions and clinical reports. Peer-reviewed articles cover topics in oncology, trauma, gastrointestinal, vascular, and transplantation surgery. The journal also publishes papers from the meetings of its sponsoring societies, the Society of University Surgeons, the Central Surgical Association, and the American Association of Endocrine Surgeons.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


