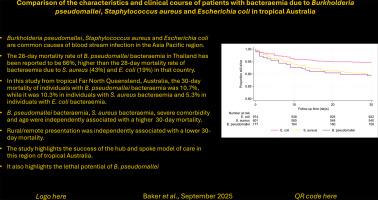
Comparison of the characteristics and clinical course of patients with bacteraemia due to Burkholderia pseudomallei, Staphylococcus aureus and Escherichia coli in tropical Australia
IF 2.5
3区 医学
Q2 PARASITOLOGY
引用次数: 0
Abstract
Background
Burkholderia pseudomallei, Staphylococcus aureus and Escherichia coli are common causes of bacteraemia in the tropical Asia Pacific region. The 28-day mortality rate of B. pseudomallei bacteraemia in Thailand has been reported to be 66%, higher than the 28-day mortality rate of bacteraemia due to S. aureus (43%) and E. coli (19%) in that country. Individuals living in rural and remote locations in these Thai studies had an even poorer prognosis. The mortality rates of individuals with bacteraemia due to B. pseudomallei, S. aureus and E. coli in countries with well-resourced health systems like Australia have not been compared directly.
Methods
We examined all cases of bacteraemia due to B. pseudomallei (between 2016 and 2022) and S. aureus and E. coli (between 2016 and 2020) in the Far North Queensland region of tropical Australia. We compared the characteristics and clinical course of these patients. We also examined the contribution of age, gender, comorbidity, remote residence and First Nations Australian status to the patients’ 30-day mortality.
Results
In total there were 177 (10.1%) episodes of bacteraemia due to B. pseudomallei, 601 (34.3%) due to S. aureus and 974 (55.6%) due to E. coli. Individuals with B. pseudomallei bacteraemia were younger than individuals with bacteraemia due to the other pathogens (median (interquartile range) age: 58 (47–67) versus 65 (49–77), p < 0.0001), they were less likely to live remotely (67/177 (37.9%) versus 730/1575 (46.4%), p = 0.03) and they did not have a greater rate of severe comorbidity (Charlson Comorbidity Index ≥ 5; 59/177 (33.3%) versus 624/1572 (39.7%), p = 0.10). There were 133/1752 (7.6%) who died within 30 days, which included 19/177 (10.7%) with B. pseudomallei bacteraemia, 62/601 (10.3%) with S. aureus bacteraemia and 52/974 (5.3%) with E. coli bacteraemia. In multivariate analysis that included all 5 pre-specified patient characteristics, the year of presentation and the 3 pathogens (with E.coli as the reference), B. pseudomallei bacteraemia (hazard ratio (HR) (95% confidence interval (CI): 2.52 (1.48–4.31), p = 0.001), S. aureus bacteraemia (HR (95% CI): 2.47 (1.69–3.59), p < 0.0001), severe comorbidity (HR (95% CI): 2.53 (1.66–3.85), p < 0.0001) and age (divided by 10) (HR (95% CI): 1.19 (1.06–1.34), p = 0.001) were independently associated with a higher 30-day mortality, while a rural/remote presentation (HR (95% CI): 0.53 (0.37–0.78), p = 0.001) was independently associated with a lower 30-day mortality. Among patients with B. pseudomallei bacteraemia, there was no association between any other of the pre-specified patient factors and 30-day mortality.
Conclusions
A well-resourced hub and spoke model of health care was able to minimise the 30-day mortality of individuals with B. pseudomallei, S. aureus and E. coli bacteraemia in this region of remote tropical Australia. However, B. pseudomallei bacteraemia had a higher 30-day mortality than bacteraemia due to S. aureus or E. coli, highlighting the lethal potential of the organism.
澳大利亚热带地区假马氏伯克氏菌、金黄色葡萄球菌和大肠杆菌所致菌血症的特点及临床病程比较
背景:假玛利氏伯克氏菌、金黄色葡萄球菌和大肠杆菌是亚太热带地区血液感染的常见原因。据报道,泰国假芽孢杆菌菌血症28天死亡率为66%,高于该国金黄色葡萄球菌菌血症28天死亡率(43%)和大肠杆菌菌血症死亡率(19%)。在这些泰国研究中,生活在农村和偏远地区的个体预后更差。在澳大利亚等卫生系统资源充足的国家,因假杆菌、金黄色葡萄球菌和大肠杆菌引起的血液感染个体的死亡率尚未进行直接比较。方法:我们对澳大利亚热带昆士兰州远北地区(2016年至2022年)、金黄色葡萄球菌和大肠杆菌(2016年至2020年)引起的菌血症病例进行了调查。我们比较了这些患者的特点和临床病程。我们还研究了年龄、性别、合并症、偏远居住地和澳大利亚原住民身份对患者30天死亡率的影响。结果:共发生假芽孢杆菌菌血症177例(10.1%),金黄色葡萄球菌菌血症601例(34.3%),大肠杆菌菌血症974例(55.6%)。假芽孢杆菌菌血症患者比其他病原体引起的菌血症患者更年轻(年龄中位数(四分位数范围):58岁(47-67岁)vs 65岁(49-77岁))。结论:在澳大利亚偏远的热带地区,资源丰富的中心辐射型卫生保健模式能够将假芽孢杆菌、金黄色葡萄球菌和大肠杆菌菌血症患者的30天死亡率降至最低。然而,假芽孢杆菌菌血症的30天死亡率高于金黄色葡萄球菌或大肠杆菌引起的菌血症,这突出了该生物的致命潜力。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Acta tropica
医学-寄生虫学
CiteScore
5.40
自引率
11.10%
发文量
383
审稿时长
37 days
期刊介绍:
Acta Tropica, is an international journal on infectious diseases that covers public health sciences and biomedical research with particular emphasis on topics relevant to human and animal health in the tropics and the subtropics.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


